This article was co-authored by Trudi Griffin, LPC, MS and by wikiHow staff writer, Jessica Gibson. Trudi Griffin is a Licensed Professional Counselor in Wisconsin specializing in Addictions and Mental Health. She provides therapy to people who struggle with addictions, mental health, and trauma in community health settings and private practice. She received her MS in Clinical Mental Health Counseling from Marquette University in 2011.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 14,747 times.
If you're taking psychotropic medications and develop feelings of restlessness, don't simply dismiss the changes. Akathisia is a side effect of medication that's characterized by depression, anxiety, and the need constantly move. If you feel like you can't control your movements and are struggling emotionally, it's vital that you work with your doctor to adjust your current medications. Your doctor may prescribe medications to treat the akathisia or recommend relaxation therapies.
Steps
Recognizing Akathisia
-
1Watch for changes in your behavior. One of the difficult things about recognizing akathisia is that the signs are similar for other conditions such as depression, anxiety, or psychosis. If you notice any of these behavioral changes, talk with your doctor or get emergency help:[1]
- Tension
- Panic
- Irritability
- Impatience
- Impulsivity
-
2Get immediate help if you have suicidal urges. Suicidal thoughts, impulsive behavior, and violent tendencies are signs of severe akathisia. If you experience any of these, immediately contact emergency services or go to the emergency room.
- If you're with a friend or family member, tell them that you don't feel safe and need to get emergency help right away.
Advertisement -
3Pay attention physical feelings of restlessness. Although there are no clear criteria for diagnosing akathisia, one of the most common signs is a feeling of restlessness. You may have akathisia if you feel as though you need to be constantly moving.[2]
- For example, people experiencing akathisia may pace over the same spot, stand up and sit down repeatedly, rock back and forth, or shift their weight from foot to foot.
-
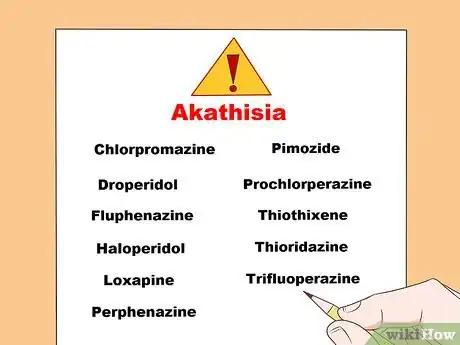
4List the psychotropic medications you're taking. Pharmacists and doctors agree that akathisia is a side effect of some medications, especially neuroleptics, selective serotonin reuptake inhibitors (SSRIs), and first-generation antipsychotics. Write down a list of medications you're on so you can give it to medical personnel if needed. Keep in mind that these medications may increase your risk for akathisia:[3]
- Chlorpromazine
- Droperidol
- Fluphenazine
- Haloperidol
- Loxapine
- Perphenazine
- Pimozide
- Prochlorperazine
- Thiothixene
- Thioridazine
- Trifluoperazine
-
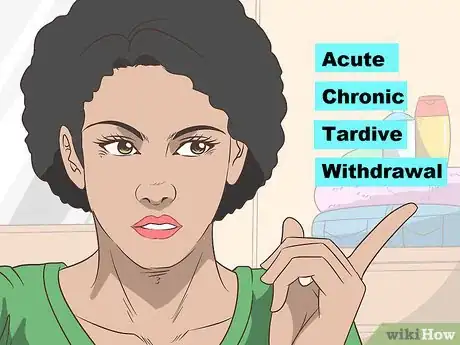
5Monitor changes during the entire course of your treatment. Akathisia can develop right after you've started some medications, once you've been taking treatments for a while, or after you've stopped or switched medications. It's important to constantly look for signs of akathisia. Akathisia is usually classified as:[4]
- Acute, if it develops after you started medication and it lasts less than 6 months.
- Chronic, if it lasts more than 6 months.
- Tardive, if it isn't related to changes in your medication and starts after you've been taking medication for several months.
- Withdrawal, if it appears within 6 weeks of switching or stopping medications.
Reducing Symptoms of Akathisia
-
1Contact your doctor as soon as you recognize signs of akathisia. If you've tracked any troubling changes in your behavior or experienced any feelings of physical restlessness, contact your doctor. Explain your concern and list the medications you're taking. The doctor may observe you or use a scale to rate your symptoms.
- Be sure to include any vitamins, herbs, or supplements you are taking when you relate your current medication regimen to your doctor. Some of these may interact unfavorably with your medications, causing akathisia.
-
2Work with your doctor to adjust your current medications. The first thing the doctor will do is to change the medications you're taking that are causing the akathisia. This might include reducing the dosage or switching to lower potency antipsychotics. Your doctor will need to closely monitor you during these transitions so you don't experience a psychotic relapse or develop withdrawal akathisia.[5]
- For example, if your akathisia is believed to be caused by a first-generation antipsychotic, the doctor may slowly switch you to a second-generation antipsychotic.
- Depending upon your symptoms when you are not on your medication, you and your doctor may decide that the benefits of staying on a given medication with akathisia outweigh the risks of going off it.
-
3Take anti-akathisia treatments. To treat the behavioral changes and feelings of restlessness, the doctor may prescribe beta-blockers or 5-HT2a receptor antagonists. If these aren't effective, the doctor can prescribe anticholinergics, benzodiazepines, amantadine, or clonidine. Your doctor may also try newer therapies which include:[6]
- Medications to increase dopamine
- Medications such as ropinirole, gabapentin, pregabalin that increase the neurotransmitter GABA
- Vitamin B6
-
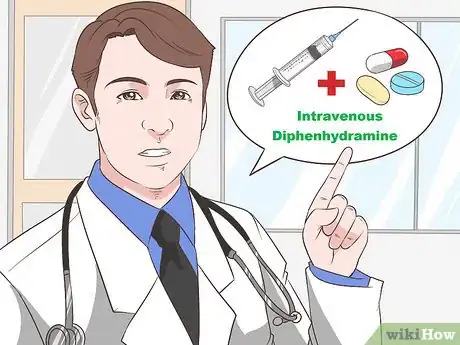
4Discuss intravenous diphenhydramine, if you'd been taking prochlorperazine. You may have read that antihistamine allergy medications can treat akathisia. Studies have shown that an intravenous drip of diphenhydramine can treat acute akathisia. Talk with your doctor about adding this as part of your treatment plan if you've been taking the antipsychotic prochlorperazine.[7]
- It's important to partner with your doctor to create a treatment plan which balances your other medications.
-
5Try professional relaxation therapies. Although more research is needed, professional relaxation treatment seems to be an effective way to treat akathisia. Performing breathing and tension relaxation therapies with trained therapists can relieve feelings of restlessness.[8]
- Research showed that although people benefited from professional relaxation treatment, the test subjects had difficulty performing the relaxation techniques on their own.
- If you think you can do a regular relaxation program at home, try yoga or meditation.
References
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK519543/
- ↑ https://www.racgp.org.au/afp/2017/may/beyond-anxiety-and-agitation-a-clinical-approach-to-akathisia/
- ↑ https://www.uspharmacist.com/article/drug-induced-movement-disorders-a-primer
- ↑ https://www.mdedge.com/psychiatry/article/89620/somatic-disorders/akathisia-restlessness-primary-condition-or-adverse-drug
- ↑ https://www.mdedge.com/psychiatry/article/89620/somatic-disorders/akathisia-restlessness-primary-condition-or-adverse-drug
- ↑ https://www.binasss.sa.cr/set/Art07.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/15028322
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2877608/