This article was co-authored by Chris M. Matsko, MD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
This article has been viewed 34,938 times.
Tetanus is a serious bacterial infection that affects your nervous system, often leading to painful muscle contractions, especially of the neck and jaw — which is why it's referred to as "lockjaw."[1] The Clostridium tetani bacteria (which produce toxin) are found in animal feces and soil, so infections usually start from puncture wounds of the legs or arms. The condition can interfere with your ability to breathe and, if left untreated, can be fatal. There is a preventative vaccine for tetanus, but no cure. If you have tetanus, you must be treated in a hospital — treatment focuses on managing and combating symptoms until the effects of the tetanus toxin resolve.
Steps
Getting Medical Treatment
-
1Go to the hospital. In addition to stiffness and spasms in the neck and jaw muscles, tetanus also causes abdominal and spinal tightness/cramping, widespread muscle twitching, difficulty swallowing, fever, sweating and rapid heart rate. If you have symptoms of tetanus, you will need to be treated in a hospital — it is a serious infection that cannot be treated at home.[2]
- Tetanus symptoms can appear anytime from a few days to several weeks after the bacteria enter your body — often through a puncture wound of the foot, such as stepping on a contaminated nail.
- The doctor will rely on a physical exam, as well as a medical and immunization history, to diagnose tetanus. No lab or blood tests are helpful to detect tetanus.
- Diseases that cause similar symptoms to tetanus that your doctor will want to rule out include meningitis, rabies and strychnine poisoning.
- The medical staff will need to clean the wound as well, removing any debris, dead tissue, and foreign objects.[3]
-
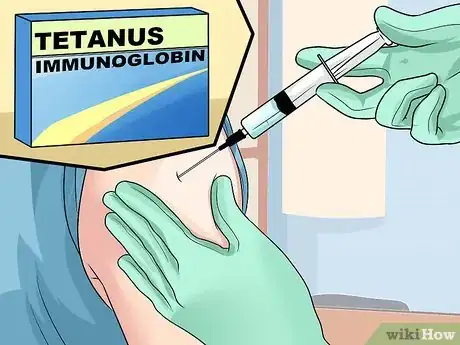
2Get a shot of tetanus antitoxin. Depending on the time between your injury and when you start to show obvious symptoms, your doctor may give you a tetanus antitoxin injection, such as tetanus immune globulin.[4] This is not a cure, however, and can only neutralize "free" toxins that have not bonded to nerve tissue. Any toxins that have already bonded to nerve tissue will not be affected.
- As such, time is of the essence. The sooner you get to the doctor (once you notice symptoms) the more effective the immunoglobulin will be in preventing the severity of symptoms.
- You will be given a dose of 3000 to 6000 units intramuscularly as soon as the diagnosis of tetanus is made. In countries in which IG is not available, equine antitoxin is used.
- Don't wait for symptoms. If you get a deep injury (such as a puncture wound) from something sharp that appears contaminated with soil, rust, feces or other debris, then clean the wound and get a tetanus shot shot from your doctor or an urgent care clinic as a preventative strategy.
Advertisement -
3Be prepared to take antibiotics. Antibiotics kill bacteria, including C. tetani, but the problem with tetanus has more to do with the toxin produced by the bacterial spores. The powerful toxin produced by the bacterial spores (once in your body) causes the vast majority of symptoms because it attaches to nerve tissue and causes excitation, which explains the widespread muscle contractions and spasms.[5]
- If you catch tetanus in its early stages, then antibiotics can be effective because they can kill the bacteria before they release much toxin.
- If your condition is advanced, antibiotics may be relatively useless, so their potential side effects may not outweigh possible benefits.
- You will be given IV antibiotics. Metronidazole 500 mg every six to eight hours is the preferred treatment for tetanus. Treatment will last seven to ten days.
-
4Expect to be given muscle relaxers or sedatives. The symptoms associated with tetanus that are often most noticeable and potentially fatal are severe muscle contractions — referred to by doctors as tetany. If tetany strikes the muscles needed for breathing, then death is likely, so taking strong muscle relaxers (such as metaxalone or cyclobenzaprine) can be life saving as well as helpful to relieve the pain associated with spasms.
- Muscle relaxers don't impact tetanus bacteria or toxin directly, but they can reduce the impact that the excited nerves have on muscle fiber contraction.
- Tetany can be so powerful that it causes muscle tears and avulsion fractures — where contracting tendons rip away bone.
- Sedatives, such diazepam (Valium), are also helpful in relieving muscle spasms, as well as the anxiety and increased heart rate associated with moderate-to-severe cases of tetanus.[6]
-
5Prepare for supportive care. If your case is severe, you may need breathing assistance with an artificial respirator machine or ventilator.[7] Even if the tetanus toxin doesn't affect your breathing muscles too badly, you may still need a breathing ventilator if you're on strong sedatives, since they often trigger shallow breathing.
- In addition to airway obstruction and respiratory arrest (the most common reason people with tetanus die), other possible complications that can occur include: pneumonia, heart failure, brain damage and bone fractures (the ribs and spine are most common).
-
6Ask your doctor about other potentially helpful medications. There are some other drugs sometimes used to ease the symptoms of tetanus, such as magnesium sulfate (reduces muscle spasms), certain beta blockers (helps regulate heartbeat and breathing) and morphine (strong sedative and painkiller).[8]
Reducing the Risk of Developing Tetanus
-
1Get vaccinated. Tetanus is preventable by getting immunized (vaccinated). In the U.S., virtually all infants get vaccinated with a series of DTaP shots, which contain protective antibodies against diphtheria, tetanus and pertussis. However, protection generally lasts only about 10 years against tetanus infection, so booster shots are needed in early and later adulthood.[9]
- In the U.S., tetanus boosters are recommended every 10 years, starting at the age of 19.
- People who get tetanus usually get vaccinated as part of their treatment because getting the condition does not provide immunity from it in the future.
-
2Quickly treat wounds. Cleaning and disinfecting any deep wound, especially punctures of your feet), is important to kill any C. tetani bacteria and prevent them from producing toxin in your body. After the bleeding has stopped, thoroughly rinse your wound with clean water or saline solution if you have any. Then clean the wound with some antibacterial alcohol-based sanitizer before covering it up with a clean bandage.[10]
- Antibiotic creams, such as Neosporin and Polysporin, also work well. They don't promote faster healing, but they discourage bacterial growth and infection.
- Change your dressing / bandage regularly, at least once a day or whenever it gets wet or dirty.
-
3Wear appropriate footwear. Most cases of tetanus develop due to stepping on something sharp that's covered in animal feces or contaminated dirt that contains spores of C. tetani bacteria — nails, glass and splinters, for examples. As such, wearing sturdy footwear with thicker soles, especially while on farms or in rural areas, is a good preventative strategy.
- Always wear flip-flops or sandals when walking on the beach and wading into shallow water.
- Don't forget to also protect your hands when working outdoors or in shops. Wear thicker gloves made from leather or a similar material.
Warning
- Without vaccination or any kind of medical treatment, about 25% of infected people die, particularly people with weakened immune systems (newborns, the elderly and those with chronic illnesses).
- If you have signs and symptoms of tetanus, do not attempt to treat it at home. Tetanus is a serious infection that requires treatment in a hospital.
References
- ↑ http://www.mayoclinic.org/diseases-conditions/tetanus/basics/definition/con-20021956
- ↑ https://www.cdc.gov/tetanus/index.html
- ↑ http://www.mayoclinic.org/diseases-conditions/tetanus/diagnosis-treatment/treatment/txc-20200893
- ↑ http://www.mayoclinic.org/diseases-conditions/tetanus/basics/treatment/con-20021956
- ↑ https://www.mayoclinic.org/diseases-conditions/tetanus/diagnosis-treatment/drc-20351631
- ↑ http://www.mayoclinic.org/diseases-conditions/tetanus/basics/treatment/con-20021956
- ↑ https://www.mayoclinic.org/diseases-conditions/tetanus/diagnosis-treatment/drc-20351631
- ↑ http://www.mayoclinic.org/diseases-conditions/tetanus/basics/treatment/con-20021956
- ↑ https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html
















-Step-11.webp)














































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...