This article was medically reviewed by Jonas DeMuro, MD and by wikiHow staff writer, Jessica Gibson. Dr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons (ACS) Fellow.
There are 16 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 25,190 times.
You've probably heard of arthritis, but may not be as familiar with gout, an arthritic disorder. Also called gouty arthritis, gout is a painful disorder caused by high levels of uric acid in the tissues, joints, and blood. If you have gout, your body produces either too much uric acid or it doesn't excrete uric acid efficiently. Your doctor can work with you to treat gout with medication. You can also try to reduce your risk factors in order to treat gout and manage pain.[1]
Steps
Medication Options
-
1Talk with your doctor about your current medications. Several medications may increase your risk for gout. Immediately consult with your physician if you take any of the following:[2]
- Thiazide diuretics (frequently used to treat edema and hypertension)
- Low-dose aspirin
- Immunosuppressant drugs
- Anti-rejection medication (such as cyclosporine and tacrolimus) following an organ transplant
-
2Use allopurinol or febuxostat. Your doctor may prescribe a medication like allopurinol or febuxostat. These medications work to block the production of uric acid, which can cause gout. Your doctor may prescribe these if you have several attacks a year or if the attacks are painful.[3]
- Febuxostat may cause changes to your liver enzymes. Allopurinol can cause skin rashes, anemia, and sometimes increased joint pain.[4]
Advertisement -
3Take probenecid. You might get a prescription for probenecid, which increases the excretion of uric acid and can reduce complications from gout. This medication helps your kidneys remove uric acid, but it means that you'll have more uric acid in your urine. This can cause other health issues like kidney stones, stomach aches, or rashes. Always follow your doctor's dosing recommendations.[5]
- Side effects of probenecid include headaches, joint pain, and rapid breathing.[6]
-
4Use a prescribed nonsteroidal anti-inflammatory drug (NSAIDS). To deal with serious attacks of gout, your doctor may want you to take an NSAIDS like indomethacin or celecoxib.[7]
- Prescription NSAIDS can cause bleeding, ulcers, or stomach pain. Make sure to follow your doctor's dosing recommendation.
-
5Take an over-the-counter pain reliever. Talk with your doctor about taking over-the-counter OTC non-steroidal anti-inflammatory drugs like ibuprofen or naproxen sodium. Your doctor might want you to take an OTC medication after you've taken higher dosage NSAIDS. This combination can stop an attack of gout.[8]
- You'll probably be prescribed 800 mg of ibuprofen to be taken three to four times a day. OTC medications are usually used only during an attack, so stop taking them after your symptoms clear up.[9]
Dietary Changes
-
1Cut back on purine-rich foods. Your body breaks down purine in food to produce uric acid which contributes to gout pain. Either avoid purine-rich food or limit your servings to two to four servings a week. If you've had kidney stones that contain uric acid or currently have an episode of gout, avoid purine-rich food completely. Foods rich in purine include:[10]
- Alcohol
- Sugary soft drinks
- Fatty foods such as fried foods, butter, margarine, and high-fat dairy products
- Organ meats. These foods have the highest levels of purines.
- Beef, chicken, pork, bacon, veal, venison
- Anchovies, sardines, herring, mussels, codfish, scallops, trout, haddock, crab, oyster, lobster, shrimp
-
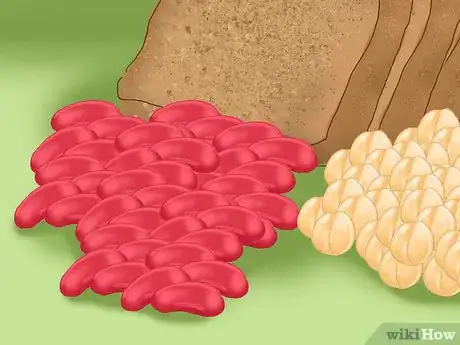
2Eat foods that lower your uric acid levels. Some foods can protect against high uric acid levels. Try to eat foods rich in phytate which can prevent kidney stone formation, including kidney stones with uric acid. To get phytate, eat two to three servings of beans, legumes, and whole grains every day. The following foods are also helpful in treating gout and kidney stones:[11]
- Calcium-rich foods, including low-fat dairy products
- Tart cherry juice: Drink three to four 8-ounce glasses of organic juice every day for relief within 12 to 24 hours.
-
3Take a supplement. There are several supplements that are recommended to treat gout. Consider taking omega-3 fatty acids (especially EPA), bromelain (which acts as an anti-inflammatory), or the B vitamin folate, quercitin, or Devil's Claw (all of which reduce uric acid levels). Take the supplements according to the manufacturer's dosing recommendations and always talk to your doctor before supplementing.[12] Some supplements may interfere with medication.
- Bromelain is an enzyme that comes from pineapples and is often used to treat digestive issues.
- Anyone with gout should avoid supplemental Vitamin C or niacin. Both of these vitamins may increase uric acid levels.
-
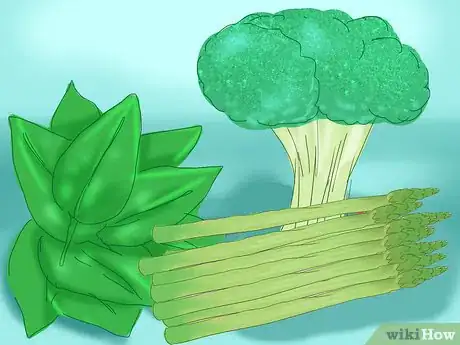
4Eat more vegetables. While you may be cutting a lot of foods out of your diet, don't forget to add healthy foods. Eat plenty of vegetables to get a variety of health benefits and nutrients.[13] While some vegetables (like asparagus, spinach, and mushrooms) contain purines, studies have shown they do not increase your chances of gout.[14]
- Eating healthy is an important part of maintaining a healthy weight. Losing weight or maintaining a healthy weight can keep your uric acid levels low.
Signs and Symptoms
-
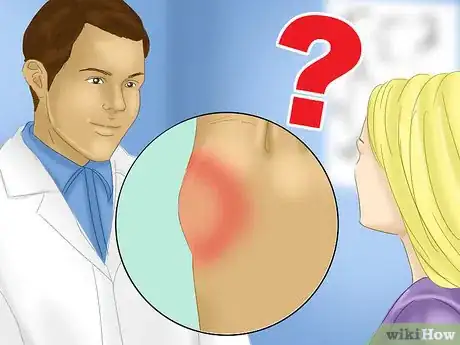
1Watch for gout symptoms. Don't be surprised if symptoms appear suddenly. They often occur at night. Symptoms are usually the most painful within the first 4 to 12 hours after the initial attack. These symptoms include:[15]
- Intense joint pain: in feet (often at the base of the big toe), ankles, knees, or wrists
- Joint discomfort after the initial attack
- Redness and other signs of inflammation, like warmth, swelling, and tenderness
- Difficulty moving the affected joint
-
2Consider your risk for gout. There are some risk factors you can't control, like a family history of gout or the prevalence of gout in adult men and postmenopausal women. But, you can control other risk factors like being overweight (or obese), untreated high blood pressure, diabetes, metabolic syndrome, and heart and kidney disease.[16] [17]
- Recent surgery or trauma also increases your risk for gout.
-
3Get a diagnosis of gout. If you are unsure whether you have gout, talk with your doctor. Your doctor will make a diagnosis based on your symptoms and medical history. Further testing and lab work might be needed.[18]
References
- ↑ http://www.jasmedical.com/patient_education/gout.pdf
- ↑ https://www.mountsinai.org/health-library/report/gout
- ↑ https://www.cdc.gov/arthritis/basics/gout.html
- ↑ http://www.drugs.com/sfx/febuxostat-side-effects.html
- ↑ https://www.hopkinsarthritis.org/patient-corner/drug-information/probenecid/
- ↑ https://www.drugs.com/sfx/probenecid-side-effects.html
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ https://www.cdc.gov/arthritis/basics/gout.html
- ↑ http://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ https://www.arthritis.org/health-wellness/healthy-living/nutrition/healthy-eating/which-foods-are-safe-for-gout
- ↑ Pizzorno, JE., Murray, MT., Joiner-Bey, H. The Clinician’s Handbook of Natural Medicine, 2002, pg. 202-208.
- ↑ Pizzorno, JE., Murray, MT., Joiner-Bey, H. The Clinician’s Handbook of Natural Medicine, 2002, pg. 202-208.
- ↑ https://my.clevelandclinic.org/health/treatments/22548-gout-low-purine-diet
- ↑ http://www.arthritis.org/about-arthritis/types/gout/articles/low-purine-diet.php
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ http://www.jasmedical.com/patient_education/gout.pdf
- ↑ https://www.cdc.gov/arthritis/basics/gout.html
- ↑ https://www.hss.edu/conditions_gout-risk-factors-diagnosis-treatment.asp#diagnosed
- ↑ http://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout
- ↑ https://medlineplus.gov/druginfo/meds/a682711.html






























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...