This article was medically reviewed by Troy A. Miles, MD. Dr. Miles is an Orthopedic Surgeon specializing in Adult Joint Reconstruction in California. He received his MD from the Albert Einstein College of Medicine in 2010, followed by a residency at the Oregon Health & Science University and fellowship at the University of California, Davis. He is a Diplomat of the American Board of Orthopaedic Surgery and is a member of the American Association of Hip and Knee Surgeons, American Orthopaedic Association, American Association of Orthopaedic Surgery, and the North Pacific Orthopaedic Society.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 30,079 times.
Gout can be confused with a number of other conditions, including pseudogout, septic arthritis, rheumatoid arthritis, and osteoarthritis. If you are concerned that you may have gout, your doctor will examine your signs and symptoms. He will also perform diagnostic tests to determine if your condition is in fact gout.
Steps
Assessing Signs and Symptoms
-
1Tell your doctor about how it began. One of the things to be aware of is that gout has a characteristic onset. It typically begins with sudden, severe pain — often in one joint, and most commonly in your big toe (on one side or the other). It often begins at night, and may wake you from sleep. The affected joint often appears red and swollen and may feel warm to the touch, and you will likely have a decreased range of motion around the affected joint.[1]
- If your joint pain is of gradual onset and does not match the profile above, it is less likely to be gout.
- It may be something else, such as rheumatoid arthritis or osteoarthritis, among other things.
-
2Consider that it may be a joint infection. One of the important diagnoses for your doctor to rule out is the possibility of an infected joint (or "septic arthritis"), which may have a presentation very similar to gout. An infection may also occur concurrently alongside a gout attack, and the two are almost impossible to tell apart without diagnostic tests.[2]
- An infected joint will likely also be sudden in onset, appear red and swollen and warm to the touch, and may be accompanied by a fever.
- You will need analysis of your joint fluid to distinguish between gout and an infection.
Advertisement -
3Be aware of the possibility of "pseudogout." Pseudogout, also known as calcium pyrophosphate deposition (CPPD), also presents very similarly to gout (hence its name). Again, the only way to truly differentiate pseudogout from gout is to have your joint fluid looked at under a microscope.[3]
-
4Take note of whether your joint self-resolves. An acute gout attack should resolve on its own within three to 10 days (although medical treatment may help to ease the symptoms during this time, to speed up recovery, and to prevent future gout attacks). If you do have gout, you will experience "attacks" of it followed by remissions (or followed by total resolution). Gout does not tend to be a persistent, chronic, and consistent condition. Rather, it either comes as a one-time attack, or a series of flare-ups and exacerbations, followed by periods of remission (or improvement).[4]
- If the pain in your joint persists for weeks or even months, without much variability, it is likely to be another diagnosis such as rheumatoid arthritis or osteoarthritis.
-
5Inform your doctor if you have a personal history of gout, a family history of gout, or other risk factors for gout. Needless to say, if you have had gout in the past, your likelihood of having a recurrent attack is significantly higher; therefore, if you have a past history of gout, your current episode is much more likely to be gout as well (as opposed to being a totally new diagnosis affecting your joint).[5]
- If your family members have had gout before, you are also at a heightened risk of developing gout. This, again, would increase the probability that your current joint problem is gout-related.
- Additional risk factors for gout include: being male, being a post-menopausal female, having other health conditions (namely high blood pressure, diabetes, or kidney problems), consuming excess alcohol, being overweight, and taking certain medications (such as aspirin, diuretics, and certain immunosuppressive agents).
-
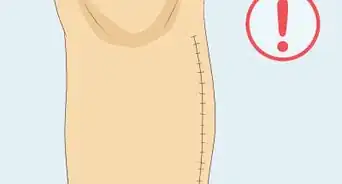
6Examine for the presence of tophi. In addition to acute (short-term) gout attacks, there are also people who suffer from chronic gout. Chronic gout consists of recurrent gout attacks over a prolonged period of time. It often leads to the formation of "tophi" (hard bumps under the skin in the joint area), which is a characteristic sign of chronic gout.[6]
- The presence of tophi — that can be visually seen in a joint — is one of the cardinal signs of chronic gout (also known as "tophaceous gout").
- This is one of the best ways to distinguish gout from other chronic arthritic conditions, such as rheumatoid arthritis, because no other chronic forms of arthritis present with tophi.
-
7Observe the number of joints involved. The medical conditions to consider in the differential diagnosis will depend significantly on whether you have only one joint affected, or multiple joints affected. The differences are as follows:[7]
- If you have only one joint affected, it is more likely to be gout, pseudogout, or an infected joint.
- If you have multiple joints affected, it may still be gout or pseudogout. It may also be another condition, though, such as rheumatoid arthritis or osteoarthritis.
- Lastly, if you have multiple joints affected, the probability of an infection is slim to none (as an infection normally affects only one joint at a time).
Investigating Further
-
1Get a blood test. A blood test can assess the levels of uric acid and creatinine in your blood. Elevated uric acid levels heighten the likelihood that it is gout. Creatinine is a measure of kidney function. Poor kidney function may lead to inadequate uric acid clearance from your body, and the resulting build-up of uric acid may predispose you to gout.[8]
- Note, however, that there is no direct correlation between uric acid levels on your blood test and a diagnosis of gout.
- Many people have elevated uric acid levels, but do not ever experience clinical signs or symptoms of gout.
- Similarly, many people who do have clinical signs and symptoms of gout do not who elevated levels of uric acid.
- There is a correlation, for sure, and your likelihood of gout is increased with elevated uric acid levels, but it is not required (nor is it the exclusive criteria) in the diagnosis of gout.
-
2Get the fluid in the affected joint aspirated.[9] Your doctor may use a needle to "aspirate," or remove, some fluid from your affected joint. She will then examine this fluid under the microscope.
- If it is gout, the microscope will show the presence of uric acid crystals.
- It is is pseudogout, the microscope will show the presence of calcium pyrophosphate crystals.
- If it is septic arthritis, the microscope will show neither uric acid crystals nor calcium pyrophosphate crystals.
-
3Have the aspirated fluid sent for a culture. Although looking at synovial joint fluid under a microscope can be diagnostic of gout (if the presence of uric acid crystals is detected), it is key to understand that gout and an infection are not necessarily mutually exclusive. Therefore, even if the test comes back diagnostic for gout, an infection could still potentially be present.[10]
- Having the synovial fluid sent for a culture will examine to see if any bacteria or other microbes grow.
- If there is an infection, the culture dish will grow the microbe, which will be diagnostic for "septic arthritis" (a diagnosis that may exist alongside gout).
-
4Ask your doctor for an x-ray of the affected joint(s). An x-ray can help to distinguish between gout and other arthritic conditions such as rheumatoid arthritis, which has a distinct appearance on x-ray. An x-ray is usually sufficient for imaging; however, in some cases, an ultrasound or a CT scan may also be of help in assessing your underlying joint problem, particularly if it does not appear to be caused by gout.[11]
Treating Gout
-
1Use NSAIDs for symptomatic relief and to decrease inflammation. If you are indeed diagnosed with gout, your doctor will likely advise you to begin taking nonsteroidal anti-inflammatory drugs (NSAIDs). Examples include Ibuprofen (Advil, Motrin) and Naproxen (Aleve). These can be purchased over-the-counter at your local pharmacy or drugstore.[12]
- Stronger NSAIDs may be prescribed to you by your doctor if the over-the-counter versions are insufficient to help relieve your gout.
-
2Try Colchicine. Colchicine is a medication that is uniquely effective at decreasing the pain caused by gout; however, when taken in high doses (which are usually required to combat an acute gout attack), the side effects of nausea, vomiting, and/or diarrhea are often too much to handle.[13]
- As a result, colchicine is most frequently used after an acute gout attack subsides, with the goal of preventing future gout attacks.
- Taken in low doses for preventative purposes, the side effects of colchicine are rarely problematic.
-
3Opt for corticosteroids. Corticosteroids are a method of inflammation control (and subsequent pain relief) for those who cannot tolerate NSAIDs and/or Colchicine. Corticosteroids can be prescribed in pill form, or they can be injected directly into the affected joint (which is usually the better option, as you avoid the side effects that can come from taking them in pill form).[14]
- An example of a corticosteroid is Prednisone.
- Corticosteroids are generally given in limited amounts, such as one (or minimal) injections into your affected joint, and/or a limited course of corticosteroids taken in pill form.
-
4Take medication to prevent future gout attacks. In addition to treating an acute gout attack (or gout exacerbation, if you suffer from chronic gout), your doctor may offer you preventative medications. The purpose of these medications is to decrease your likelihood of future gout attacks.[15]
- Allopurinol is an example of a medication that can help to prevent excess uric acid production.
- Probenecid is an example of a medication that can aid in your kidney's ability to filter and remove uric acid from your body.
References
- ↑ https://www.niams.nih.gov/health-topics/gout
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/clinical-presentation-of-gout/
- ↑ https://my.clevelandclinic.org/health/diseases/4756-calcium-pyrophosphate-dihydrate-deposition-disease-cppd-or-pseudogout
- ↑ https://www.cdc.gov/arthritis/basics/gout.html
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/gout
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/clinical-presentation-of-gout/
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ https://emedicine.medscape.com/article/329958-overview
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/clinical-presentation-of-gout/
- ↑ https://emedicine.medscape.com/article/389965-overview
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ https://www.aafp.org/afp/2014/1215/p831.html


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...