This article was co-authored by Chris M. Matsko, MD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
This article has been viewed 94,416 times.
Cellulitis is a potentially serious skin and soft tissue infection that afflicts millions of people every year. While some cases of cellulitis are minor and don't require medical attention, a relatively substantial amount of cases do demand treatment by medical professionals. One of the most dangerous things about cellulitis is that it can develop quickly and turn from a local infection to a systemic infection that impacts your entire body. If you suspect you have cellulitis, you should be vigilant about monitoring it and make sure to contact a medical professional if you think it is growing beyond a local, controllable, infection.
Steps
Spotting Local Symptoms
-
1Pay attention to inflammation, redness, and warmth. These are the tell-tale sign of cellulitis. Inflammation, redness, and warmth in the affected region of your body will likely be the first signs of infection. Patients should monitor their infection closely. Consider:
- Inflammation and redness might occur after some pain at the point of infection.
- Once you notice inflammation and redness at the point of infection, you should monitor it closely as the infection can spread very quickly.
- If the infection turns from red to a purple or violet color and expands, you should see a doctor as soon as possible.[1]
-
2Observe a central area that is swollen and potentially filled with pus. A good indication of cellulitis is that we can observe a central area – the initial place of infection – that is abscessed and swollen. This initial place of infection is often filled with pus. Treatment might, in some cases, demand that the abscess is drained. [2]Advertisement
-
3Report sensitivity and pain to touch the skin. Many patients inflicted by cellulitis report sensitivity to the infected area if touched. While this sensitivity or pain might be minimal at first, it can quickly develop into a much more intense level of pain and discomfort. If your pain increases in intensity quickly, contact a medical professional.[3]
-
4Feel a heat or warmth radiating from the infected area. A common symptom of cellulitis is that the infected area is warm or even hot to the touch. At first this warmth might seem like nothing, but it can quickly escalate and cause discomfort to the patient. In addition, heat or warmth radiating from the infected area is an indication that the infection is spreading and expanding, possibly becoming systemic.[4]
Watching for Systemic Symptoms
-
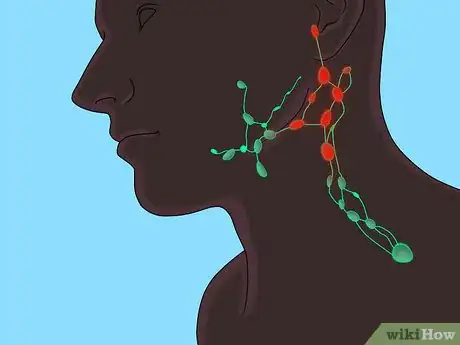
1Watch from swollen glands. Serious cases of cellulitis will spread beyond the initially infected region to become systemic and impact the rest of the body. One common sign of systemic cellulitis is swollen lymph glands. You should consider that:
- Lymph glands nearest to the infection will swell first.
- Lymph glands may become tender and exhibit pain when touched.
- Swollen lymph glands indicate that the infection is spreading well beyond the initially infected region and the patient requires immediate medical care.
- Lymph nodes are located on your neck, in your armpits, and around your groin, among other places.
-
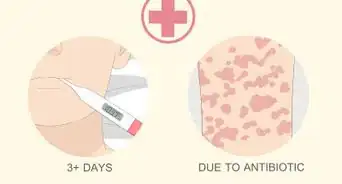
2Notice if you experience fever and/or chills. While systemic symptoms vary from patient to patient, bad cases of cellulitis can cause someone to experience a fever or chills. The fever or chills might seem to go and come with no predictability; however, the worse the infection is, the more the fever and chills will persist.
- Fever is an indication of a serious case of systemic infection.
- See your doctor immediately if your case of cellulitis is accompanied by fever and/or chills.[5]
- A doctor might advise Tylenol or other fever reducing medicines.
-
3Feel fatigued for no apparent reason. People who suffer from a serious case of cellulitis may experience fatigue for no apparent reason. They will feel tired and drained of energy. A feeling of fatigue is a systemic symptom that indicates a case of cellulitis that is expanding. Consult your doctor immediately if your cellulitis is accompanied by prolonged fatigue.
-
4Notice if you are sweating for no apparent reason. Another symptom of a serious systemic case of cellulitis is when the patient sweats for no clear reason. Sweating may or may not be accompanied by fatigue, fever, and or chills. Regardless, a case of cellulitis accompanied by sweating is an indication that the infection is expanding and affecting more than the area of initial infection.
-
5Pay attention to pain that seems more serious than the size of the infection would indicate. Many serious cases of cellulitis will have associated pain emanating from the infected area. This pain will seem much more severe than the size of the infection would suggest. If you have an infection with intense pain, you should contact a doctor immediately.
-
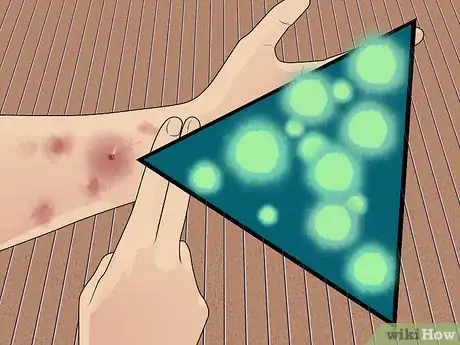
6Observe lymphangitic spread. Lymphangitic spread appears as red lines emanating outward from the infected area. If you observe this spreading, it means that your cellulitis is potentially severe. Observed spreading indicates that the infection is radiating outward and will become a systemic infection if it goes untreated.[6]
Understanding Cellulitis
-
1Treat wounds immediately to help prevent infection. Treating wounds immediately is important because cellulitis can be introduced to the body through an open wound. Any open would, however innocuous and seemingly harmless, can create an opportunity for the development of cellulitis. Inflammation generally starts at the point where skin was previously broken. As a result, you should treat all newly opened wounds as soon as possible. Introduction of cellulitis can be caused by:
- Cuts
- Blisters
- Burns
- Cracks in the skin
- Surgical wounds
- Sites of intravenous catheter insertion
-
2Recognize that cellulitis is caused by a bacterial infection. Cellulitis is most often caused by Streptococcus type A and Staphylococcus aureus; however, while these are the two most common causes, it can be caused by other types of bacteria. Blood test and cultures are needed in order to determine exactly the type of bacteria that is causing cellulitis.[7]
- If you have a known or suspected underlying condition, such as diabetes, your doctor will likely want to perform more tests.
- Be conscious of methicillin-resistant Staphylococcus aureus (MRSA), which is a bacteria that is resistant to antibiotic treatment. Oral medication will not work on this type of infection and you will need to be given vancomycin intravenously. MRSA must be treated quickly or it can become life-threatening.
-
3Take antibiotics to treat cellulitis. Treatment for mild forms of cellulitis include elevation of the affected area and treatment of the underlying conditions. Patients that have edema as one of their underlying conditions may benefit from compression stockings or diuretics. Nevertheless, antibiotics are usually the best solution to heal this type of infection. Antibiotics are used orally or intravenously depending of severity affected skin area.[8]
- For mild infections, your doctor may give you the oral antibiotic cephalexin. In more severe cases, you may be treated with vancomycin or meropenem.
- One major complication of cellulitis includes infection of deeper structures, such as bone. This can lead to a disease called osteomyelitis, which is the infection of the bone and requires aggressive treatment.
- In cases of recurrence of disease treatment with antibiotics may last up to several months.
Expert Q&A
-
QuestionDoes cellulitis present as a sunburn-like condition, with pain and eventual peeling of the skin?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician Yes, you can can have peeling of the skin with cellulitis, giving your skin the appearance of an orange peel. This is known as "peau d'orange.”
Yes, you can can have peeling of the skin with cellulitis, giving your skin the appearance of an orange peel. This is known as "peau d'orange.” -
QuestionIf my first signs of cellulitis are abdominal pain, sickness, shivers, and fever, is that normal?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician You usually do not have abdominal pain with cellulitis. You normally have tenderness and redness of the skin with increased temperature and severe inflammation. You should contact your doctor.
You usually do not have abdominal pain with cellulitis. You normally have tenderness and redness of the skin with increased temperature and severe inflammation. You should contact your doctor.
References
- ↑ https://www.nhs.uk/conditions/cellulitis/
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000855.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000855.htm
- ↑ http://kidshealth.org/en/teens/cellulitis.html
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000855.htm
- ↑ http://www.cdc.gov/mmwr/preview/mmwrhtml/00043200.htm
- ↑ https://www.cdc.gov/groupastrep/diseases-public/Cellulitis.html
- ↑ https://www.nhs.uk/conditions/cellulitis/





















-Step-11.webp)














































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...