This article was medically reviewed by Troy A. Miles, MD. Dr. Miles is an Orthopedic Surgeon specializing in Adult Joint Reconstruction in California. He received his MD from the Albert Einstein College of Medicine in 2010, followed by a residency at the Oregon Health & Science University and fellowship at the University of California, Davis. He is a Diplomat of the American Board of Orthopaedic Surgery and is a member of the American Association of Hip and Knee Surgeons, American Orthopaedic Association, American Association of Orthopaedic Surgery, and the North Pacific Orthopaedic Society.
There are 27 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 108,417 times.
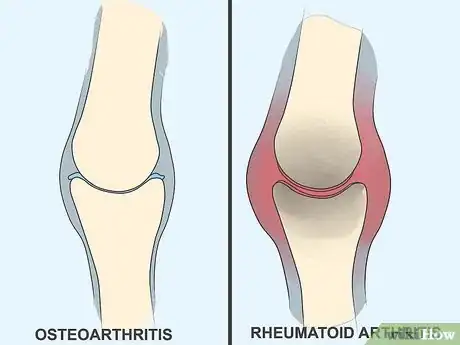
Experts say arthritis is a very common condition. It typically causes swelling or tenderness in one or more of your joints, along with pain and stiffness.[1] There are several types of arthritis, but research shows that the two most common forms are osteoarthritis and rheumatoid arthritis. Osteoarthritis occurs when the cartilage in your joint erodes away, while rheumatoid arthritis is a chronic autoimmune disorder.[2] Since arthritis can get progressively worse, it's best to seek medical treatment as soon as you recognize the symptoms. With treatment, you may be able to manage your condition.
Steps
Recognizing Early Symptoms of Arthritis
-
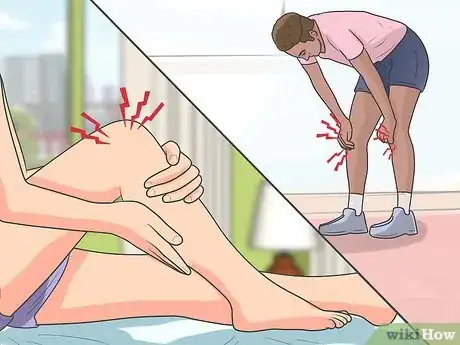
1Take notice of any joint pain. Joint pain is the most characteristic symptom of all types of arthritis.[3] You might notice the pain after exercising or using the joints extensively, which is the case with "wear and tear" arthritis (OA), or upon waking and after periods of disuse, which is more characteristic of RA.
- Arthritic pain is usually described as dull, achy and/or throbbing. The more destructive types of arthritis can also generate sharp and electric-type pain.
- Arthritic pain usually starts out mild, then progressively gets worse. The pain levels of OA gradually worsen, whereas some really inflammatory types (such as gout attacks) become extremely painful very suddenly.
-
2Look for joint swelling and redness. Although the term arthritis literally means joint inflammation, some types involve much more swelling than others. In general, the wear and tear of OA doesn't lead to much swelling or redness. In contrast, RA involves lots of swelling and redness because the body's immune system attacks the lining of the joint capsule (synovial membrane). Gout is also known for lots of inflammation due to the deposit of sharp uric acid crystals within joint capsules, particularly of the big toe.[4]
- PsA also involves the immune system attacking joints, which is why it's classified as an autoimmune disorder, so swelling and redness are more noticeable.
- RA not only causes severe inflammation in affected joints (usually of the hands and wrists), but also low-grade inflammation throughout the body.
- Not being able to remove your rings is a sign of swelling in the joints of the hands.
Advertisement -
3Watch for joint stiffness. Stiffness is another common early sign of virtually all types of arthritis.[5] It's the inability to freely move joints due to pain, swelling and/or some degree of joint destruction. Along with stiffness, you may also feel or hear creaking or cracking sounds as you move joints after periods of inactivity, especially with OA.[6]
- Initially, stiffness doesn't usually involve reduced range of motion, but it's a sign that there's a problem in the joint that will likely get worse.
- Stiffness and other symptoms usually occur on only one side of the body with OA and gout, whereas both sides are typically involved with autoimmune types, such as RA and PsA.[7]
- Stiffness is usually worse in the morning with RA and PsA, but worse at the end of the day with OA.
-
4Be aware of unusual fatigue. Fatigue (extreme tiredness) can be another early sign of some types of arthritis, but not all types.[8] The autoimmune types (RA and PsA) tend to cause inflammation and other problems throughout the body, not just individual joints. As such, the body gets fatigued and rundown from trying to combat all the inflammation. Chronic fatigue can adversely affect emotions, mood, sex drive, attentiveness, creativity and productivity.[9]
- Fatigue from RA and PsA can also be associated with poor appetite and weight loss.
- Other types of arthritis, such as OA, can trigger chronic fatigue if the joint pain is great enough to significantly affect your sleeping and eating patterns.
Recognizing Advanced Symptoms of Arthritis
-
1Be aware of reduced range of motion. As pain, inflammation, stiffness and/or damage progresses within joints, you eventually begin to lose the ability to move them normally. As such, reduced range of motion (limited movement) is a common sign of advanced arthritis and one of the main causes of disability.[10] You may not be able to bend down as far or be as flexible as you once were.
- Reduced range of motion is slow and gradual with OA, as the cartilage wears down and the bones come into contact with each other and as you form bone spurs or osteophytes.
- With RA and PsA, range of movement often depends on the degree of joint swelling, which can come and go.[11] However, with time, RA and PsA are destructive to cartilage and severely limit joint movement.[12]
- Septic arthritis is caused by an infection in the joint and is characterized by sudden, severe pain and difficulty using the affected joint. This type of infection can destroy a joint quickly — within weeks.[13]
-
2Take note of sudden weakness. Associated with progressive pain and reduced range of motion within joints is weakness. The weakness may be due more to trying to avoid pain or it may be due more to destruction of the joint's integrity. Furthermore, lack of exercise (common with arthritis sufferers) leads to loss of muscle tissue, which leads to loss of strength.[14] You may notice you can't lift as much or walk as far as you once could. Your grip strength and hand shake may not be as firm.
- Muscle atrophy (shrinking and loss of strength) is common in muscles that surround arthritic joints.
- Weak muscles and joints feel unstable and usually shake or twitch a little when put under heavy loads.
- Associated with progressive weakness is loss of agility, dexterity and coordination. If you have arthritis in your hands, you may feel clumsy and drop things often.
-
3Look for any joint deformities. Joint deformity or disfigurement eventually occurs with all forms of arthritis, although it can develop quicker and be more noticeable with certain forms. RA is notorious for severe joint deformity in the hands and feet because the inflammation leads to erosion of cartilage and bone, as well as ligament laxity (loosening).[15] Long term, RA is more destructive than virtually all other types and causes the most disability in people.
- OA can lead to joint deformity also (often described as knobby), but not the extreme crookedness characteristic of RA.[16]
- If you notice any nodules (large tender bumps) near your joints, that's likely a sign of RA. Nodules occur in 20–30% of RA cases, usually in the hands, feet, elbows and knees.[17]
-
4Watch for any skin changes. Another late-stage sign of arthritis is associated skin changes.[18] Aside from potential nodules, RA and PsA often cause characteristic changes in skin texture and color, both near painful joints and in distant locations of the body. RA tends to make the skin look more red, mainly due to swelling of small blood vessels beneath the skin's surface (called vasculitis).[19]
- In contrast, PsA usually involves psoriasis of the skin, which involves the formation of thick, silvery scales and itchy, dry, red patches.[20]
- Gout flare-ups are usually associated with crusty formations on skin near the painful joint.
- All types of arthritis that involve significant swelling and inflammation increase the heat underneath the skin and can make it feel and look more leather-like.
Distinguishing the Main Types of Arthritis
-
1Understand what OA is. Osteoarthritis (OA) is the most common type of arthritis and is caused by the gradual wearing out of joints due to overuse, obesity and/or joint injuries.[21] OA doesn't involve much inflammation and can often be managed by losing weight, switching activities/exercises that are more gentle on joints and changing your diet (less sugar and preservatives, more water and fresh produce).[22]
- OA most often affects weight-bearing joints, such as the knees, hips and spine, although OA in the hands is common also.[23]
- OA is diagnosed by a physical exam and x-rays. Wearing away of cartilage and the development of small bone spurs are characteristic of OA on x-ray.[24]
- Treatment for OA centers around lifestyle changes and either non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, or painkillers like acetaminophen.[25]
-
2Learn about RA. Rheumatoid arthritis (RA) is not nearly as common as OA, but it seems to be more prevalent compared to past decades. What causes it is a bit of a mystery, but it's assumed that the immune system gets confused and attacks joint tissues and other parts of the body by mistake — also described as an over-active immune system. RA is characterized by lots of inflammation and pain, which can come and go (called flares).[26]
- RA usually affects the body bilaterally — the same joints on both sides of the body at the same time.
- RA seems to have more of a genetic link, so if your close relatives have it, you're much more likely to develop it.[27]
- Women are much more likely to develop RA compared to men.[28]
- Unlike in OA, children can be affected by RA — called juvenile idiopathic arthritis or JIA.[29]
- RA is diagnosed by a physical exam, x-rays and a blood test. Inflammation and joint deformity are characteristic of RA on x-ray. Between 70–80% of people with RA test positive for a marker in their blood called rheumatoid factor.[30]
- Treatment for RA centers around taking strong NSAIDs, as well as disease-modifying anti-rheumatic drugs (DMARDs) and biologic response modifiers (biologics).[31]
-
3Don't confuse gout with OA or RA. Gout is caused by high levels of uric acid in the blood from having a purine-rich diet.[32] High levels of uric acid eventually precipitates out within the blood, forming sharp crystals, which get deposited in and around joints. The sharp crystals quickly create lots of inflammation and severe pain, most often in the big toe, but also in other joints of the feet, hands and limbs. Gout attacks are typically short-term (a few days or so), but can re-occur on a regular basis.[33]
- Uric acid crystals can form crusty lumps or nodules called tophi around affected joints, which can mimic RA.
- Purine-rich foods include organ meats (liver, kidneys), bacon, shellfish, sardines, anchovies, chicken and gravies. Too much beer and red wine can also trigger gout attacks.[34]
- Gout is diagnosed by a physical exam, dietary history, x-rays and a blood test. People with gout will have high levels of uric acid in their blood (called hyperuricemia).[35]
- Treatment for gout is centered on short-term use of NSAIDs or corticosteroids, as well as colchicine (Colcrys). Long-term prevention is based on dietary changes.[36]
Expert Q&A
-
QuestionWhat does osteoarthritis feel like?
 Jason Myerson, DPT, DMT, OCS, FAAOMPTJason Myerson is a Physical Therapist and a Certified Orthopedic Specialist. He is affiliated with Performance Physical Therapy & Wellness with clinics located in Connecticut. He serves as adjunct faculty in the Physical Therapy Department at Quinnipiac University. Jason specializes in helping active people get back to hobbies, activities, and sports they love while utilizing an integrated approach to wellness. He holds an MA in Physical Therapy from Quinnipiac University and a Doctorate in Physical Therapy (DPT) from Arcadia University. He is Residency and Fellowship trained in Orthopedic Manual Therapy, achieved a Doctorate in Manual Therapy (DMT) and became a Fellow of the American Academy of Orthopedic Manual Physical Therapists (FAAOMPT).
Jason Myerson, DPT, DMT, OCS, FAAOMPTJason Myerson is a Physical Therapist and a Certified Orthopedic Specialist. He is affiliated with Performance Physical Therapy & Wellness with clinics located in Connecticut. He serves as adjunct faculty in the Physical Therapy Department at Quinnipiac University. Jason specializes in helping active people get back to hobbies, activities, and sports they love while utilizing an integrated approach to wellness. He holds an MA in Physical Therapy from Quinnipiac University and a Doctorate in Physical Therapy (DPT) from Arcadia University. He is Residency and Fellowship trained in Orthopedic Manual Therapy, achieved a Doctorate in Manual Therapy (DMT) and became a Fellow of the American Academy of Orthopedic Manual Physical Therapists (FAAOMPT).
Physical Therapist & Certified Orthopedic Specialist Physical Therapist & Certified Orthopedic SpecialistExpert AnswerOsteoarthritis is a normal process that our joints and bones go through as we age. The most common symptoms of osteoarthritis are stiffness and tightness, but other symptoms can include a deep, nagging ache or sharp pains. The best way to ease this pain is with movement, like going for a walk or doing gentle exercise.
Physical Therapist & Certified Orthopedic SpecialistExpert AnswerOsteoarthritis is a normal process that our joints and bones go through as we age. The most common symptoms of osteoarthritis are stiffness and tightness, but other symptoms can include a deep, nagging ache or sharp pains. The best way to ease this pain is with movement, like going for a walk or doing gentle exercise.
Warning
- If you suspect you have arthritis, see your health care provider as soon as possible. Early diagnosis and disease modifying drugs can alter the course of some forms (such as rheumatoid arthritis).
References
- ↑ https://www.nhs.uk/conditions/arthritis/
- ↑ https://www.nhs.uk/conditions/arthritis/
- ↑ https://www.arthritis.org/health-wellness/healthy-living/managing-pain/understanding-pain/sources-of-arthritis-pain
- ↑ https://my.clevelandclinic.org/health/diseases/12061-arthritis
- ↑ https://www.healthdirect.gov.au/arthritis#symptoms
- ↑ https://www.nhs.uk/conditions/osteoarthritis/symptoms/
- ↑ http://www.arthritis.org/living-with-arthritis/pain-management/understanding/types-of-pain.php
- ↑ https://www.healthdirect.gov.au/arthritis#symptoms
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-fatigue-syndrome
- ↑ https://www.cdc.gov/arthritis/basics/osteoarthritis.htm
- ↑ https://www.psoriasis.org/about-psoriatic-arthritis/
- ↑ https://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-symptoms/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK538176/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435919/
- ↑ https://www.arthritis.org/diseases/more-about/joint-deformities-in-rheumatoid-arthritis
- ↑ http://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-symptoms/
- ↑ http://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-symptoms/
- ↑ http://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-symptoms/
- ↑ https://my.clevelandclinic.org/health/diseases/13290-rheumatoid-vasculitis
- ↑ https://www.psoriasis.org/about-psoriasis/
- ↑ https://www.cdc.gov/arthritis/basics/osteoarthritis.htm
- ↑ https://health.clevelandclinic.org/four-food-tips-to-improve-your-arthritis-symptoms/
- ↑ https://my.clevelandclinic.org/health/diseases/5599-osteoarthritis
- ↑ https://my.clevelandclinic.org/health/diseases/5599-osteoarthritis
- ↑ https://my.clevelandclinic.org/health/diseases/5599-osteoarthritis
- ↑ https://www.cdc.gov/arthritis/basics/rheumatoid-arthritis.html
- ↑ https://familydoctor.org/condition/rheumatoid-arthritis/
- ↑ https://familydoctor.org/condition/rheumatoid-arthritis/
- ↑ https://kidshealth.org/en/parents/jra.html
- ↑ http://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-symptoms/
- ↑ https://my.clevelandclinic.org/health/diseases/4924-rheumatoid-arthritis#management-and-treatment
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ https://www.cdc.gov/arthritis/basics/gout.html
- ↑ https://familydoctor.org/low-purine-diet/
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout#diagnosis-and-tests
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout#management-and-treatment
About This Article
One of easiest ways to recognize arthritis is to look out for a dull ache or throbbing pain in your joints, either after exercising or after a period of inactivity, such as sleeping. Similarly, watch out for any stiffness in your joints, which is another common early sign of arthritis. It is also a good idea to monitor your joints for any swelling or redness, such as difficulty removing rings, as this can be a sign of inflammation. For more guidance from our Orthopedic Surgeon reviewer, including how to distinguish between the main types of arthritis, keep reading.

































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...