This article was co-authored by Matt Garcia. Matt Garcia is an experienced phlebotomist in Vancouver, Canada. He holds a Diploma in Medical Laboratory Assistance and is certified under the British Columbia Society of Laboratory Science. He previously worked in a high-volume outpatient lab and is currently employed in an acute care hospital and Level III trauma center in downtown Vancouver.
This article has been viewed 10,025 times.
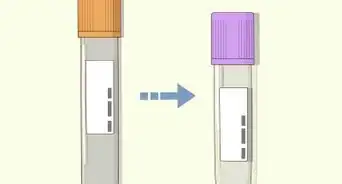
After collecting blood, the tubes must always be properly labelled to ensure positive patient and specimen identification. This is a general guide for knowing how to label a Vacutainer tube using computer-generated adhesive labels.[1] Practitioners should always refer to their facility's resources for specific procedures.
Steps
-
1Identify your patient. Ask the patient to state their first and last name and their date of birth. Confirm this information against your labels as well as the patient's hospital wristband (if inpatient) or health card (if outpatient). If using a hospital wristband, you should also match the patient's health number or medical record number (MRN) if present and if your hospital policy dictates.[2]
-
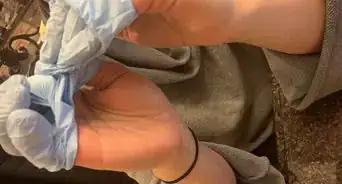
2Perform venipuncture according to your facility's protocols and procedures. As soon as the collection is over, engage the safety feature on the needle to prevent a needlestick injury. Invert all tubes to adequately mix the blood with the additives.[3]Advertisement
-
3Remain at the patient's bedside. Tubes should always be labelled immediately after venipuncture in front of the patient. Do not exit the patient's room or allow the patient to leave until all your tubes have been labelled.[4]
-
4Peel the label off its backing and stick it on your finger.
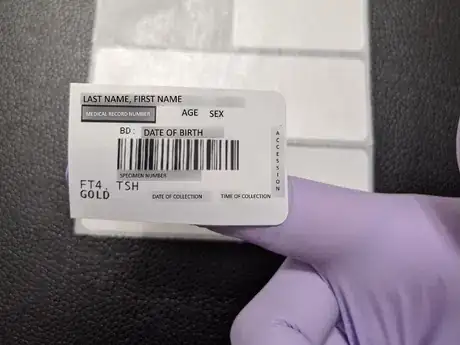
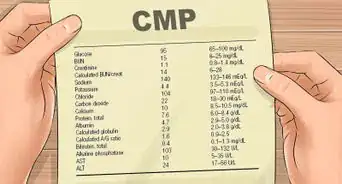
- A typical blood specimen label has the following information on it:[5]
- Patient's first and last name.
- Date of birth, age, and sex.
- MRN or health number plus the lab accession number.
- The tests to be performed on that specific sample.
- The tube colour or type, varies by facility. (In these images: LAV = lavender top EDTA; GOLD = gold top SST; LT GRN = light green PST)
- A barcode to be scanned for specimen tracking and analysis.
- A typical blood specimen label has the following information on it:[5]
-
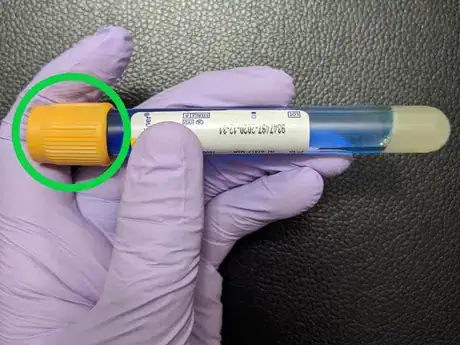
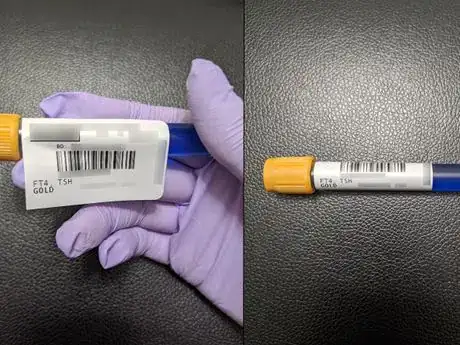
5Hold the tube horizontally so that the coloured stopper is facing left.
-
6Place the label on the tube. Ideally, the lab label should be covering the tube manufacturer label to leave a small window so the specimen is still visible. The left edge of the label should be directly against the tube stopper.[6]
- It helps to roll the tube with your hands or fingers to ensure complete adhesion.
-
7Repeat for your remaining tubes. Always label one tube at a tube.
-
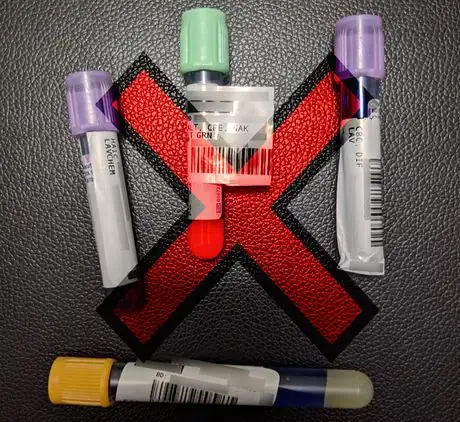
8Avoid incorrect placement or positioning. Labels should not:
- Be crooked or slanted. The barcode should be straight.
- Be wrinkled, creased, or torn.
- Be wrapped around the tube so the barcode is perpendicular, or folded over itself like a "flag".
- Be covering the specimen window, obscuring the view of the sample.
-
9Follow specific downtime procedures if IT failures prevent you from generating labels. At minimum, handwrite the patient's first and last name, MRN or health number, date of birth, time of collection in 24-hour format, and your initials or employee ID. You should write this information on a blank specimen label or on the tube manufacturer label using indelible blue or black ink.
Warnings
- The person who collects the blood sample is ultimately responsible for the accuracy of patient identification and specimen labelling. A mislabelling situation occurs when a label is placed on the wrong tube or when a specimen is labelled with a different patient's label. Because many clinical decisions are supported by lab tests, errors in labelling can have profound adverse effects on patient care and safety if left uncaught. Always take the time to ensure you have correctly identified your patient and positively matched your specimen labels.⧼thumbs_response⧽
- Never pre-label your tubes. Tubes should always be labelled after the blood has been collected.⧼thumbs_response⧽
- Be diligent in your label placement. Many lab tests are automated, and analysis might be delayed if the barcode cannot be scanned due to crookedness or wrinkles.⧼thumbs_response⧽
References
- ↑ https://www.pathology.uci.edu//services/specimen-containers.asp
- ↑ https://www.pathology.uci.edu/services/specimen-labeling-requirements.asp
- ↑ https://pathlabs.ufl.edu/client-services/specimen-shipping/blood-collection-process-venipuncture/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622200/
- ↑ https://pathlabs.ufl.edu/client-services/specimen-shipping/blood-collection-process-venipuncture/
- ↑ https://www.youtube.com/watch?v=SHSfIT2Rvyw
























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...