This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
This article has been viewed 9,377 times.
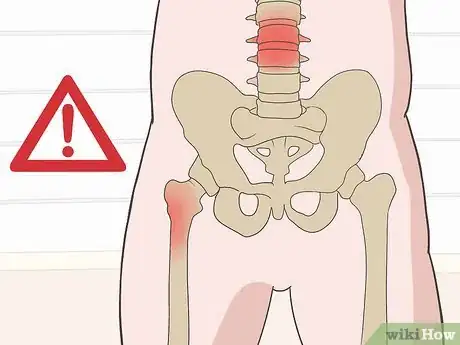
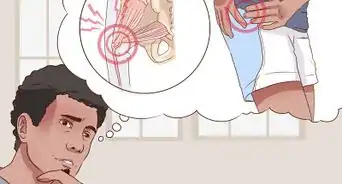
Hip bursitis—now more commonly known as greater trochanteric pain syndrome—is an inflammation of the bursa, or jelly-filled sacs, that are located within your hip. You have a bursa at each of the points of your hip bone, which is also known as the greater trochanter. When this bursa is inflamed, it’s called trochanteric bursitis. You also have a bursa located on the inner groin area of each side of your hip, which causes pain in your groin, but this condition is known as hip bursitis. The condition may also present with tendinopathy, or tendon changes from overuse. Check for common symptoms by paying attention to where and how your pain manifests. If you think you might have hip bursitis, see a doctor for a diagnosis and treatment.
Steps
Identifying Common Symptoms and Risk Factors
-
1Note whether your hip feels painful, achy, or stiff. Check for a very tender spot at the bony point of your hip. The pain may also sometimes present along your outer thigh or even in the groin area. The pain may be mild to moderate.[1]
- If it feels severely painful or if you’re having sharp, shooting pains, go to the emergency department of your nearest hospital as soon as possible.
- If you notice the pain more when rotating your leg in and away from your body, this may indicate a joint problem instead, such as arthritis.
-
2See if the pain increases when you move. Get up and walk around if you have been sitting for a while or pay attention to how your hip feels as you go about your normal activities. You may notice that the pain increases after walking, standing, running, or bicycling for a long period of time. Squatting and climbing stairs can also be painful when you have bursitis.[2]
- Even everyday activities, such was walking around your house can be more difficult when you have hip bursitis.
Advertisement -
3Apply gentle pressure to your hip to see if it’s painful. Press the bony point of your hip bone, which is known as the greater trochanter, with your fingertips. There’s a bursa located here, which may be painful when you press on it. If the point of your hip feels tender, this is a strong indication of bursitis.[3]
- You can also press on the inside and outside of your thigh to check for tender spots, but it can be harder to check the bursa in these areas.
-
4Inspect the skin over your hip for redness and swelling. Remove your clothing and inspect the painful hip area. If it looks red or swollen, this may be another sign of bursitis. However, these signs may not always be easily visible.[4]
Warning: See a doctor right away if the swelling is severe, or if you have a rash or bruising over the area.
-
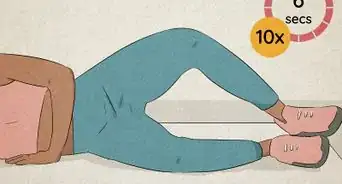
5Assess your pain level when you’re lying in bed at night. Lying in bed at night is when some people first notice bursitis since it often seems to get worse at night. Other times you might notice the pain is more intense include when you:[5]
- Stand up after sitting in a chair or car
- Get out of bed in the morning
- Turn over to the affected side
-
6Identify ways you might have exerted or injured yourself. Injuries and overuse are the most common causes of bursitis. Consider if you’ve done any form of exercise or if you’ve been injured recently to determine a potential cause. Some things that might have led to developing bursitis include:[6]
- Doing the same motion over and over again, such as taking a long bike ride or climbing stairs on a stair machine for a long time
- Falling onto your hip
- Bumping your hip into something
- Lying on your hip for a long period of time[7]
-
7Consider whether you are at a higher risk of bursitis. Older adults, such as those over 70 are more likely to get bursitis, but it may affect you if you’re younger, too. Likewise, if you have a job that requires repetitive motion involving your hips, such as squatting, lifting, or climbing stairs, you may also be at a higher risk. Your risk of developing bursitis may also be higher if you have any of the following conditions:[8]
- Bone spurs or calcium deposits
- Rheumatoid arthritis
- Gout
- Thyroid disease
- Psoriasis
- Spine diseases, such as scoliosis or lumbar arthritis
- Previous surgeries
- One leg that is longer than the other[9]
Seeking Medical Attention
-
1See a doctor immediately if you notice any severe symptoms. In some situations, hip pain may be a medical emergency and require prompt treatment. Go to the emergency department of your local hospital or call emergency services if you are: [10]
- In so much pain you can barely move
- Unable to move your joint because it is too stiff
- Severely swollen, rashy, or bruised
- Experiencing sharp or shooting pains, especially when exercising or exerting yourself
- Running a fever
-
2Have a physical exam and tell your doctor about your symptoms. During a physical exam, your doctor will inspect your hip visually and use their hands to check for tender areas. They will also ask you questions about your symptoms, such as when the pain started and if anything relieves the pain or makes it worse.[11]
- You can see your regular family doctor for this checkup, but they may refer you to an orthopedic specialist if they’re unable to make a diagnosis.
-
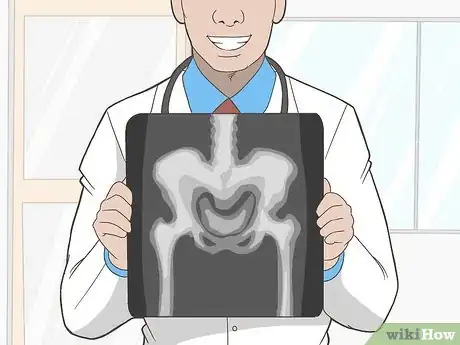
3Get imaging tests to confirm a diagnosis if needed. An X-ray, magnetic resonance imaging (MRI), or another type of imaging test is rarely required for your doctor to confirm that you have bursitis. However, they may order one of these tests to confirm an alternative diagnosis.[12]
- The type of imaging test your doctor orders will depend on what they’re checking for and how much detail is required. For example, an X-ray could show if the hip is fractured, while an MRI would reveal issues with the soft tissues in your hip and the surrounding areas as well.
- Although imaging tests can be uncomfortable, they are not painful and typically only take around 10-15 minutes to complete.
-
4Have the bursa fluid analyzed in a lab to check for an infection. In some very rare cases, bursitis can be caused by an infection of the fluid in the bursa. If your doctor suspects this is what’s causing the pain in your hip, a specially trained orthopedist or rheumatologist may need to collect a sample using a needle and send it for laboratory testing. However, this test is rarely done because it poses a high risk of joint infection from penetrating and aspirating the bursa.[13]
Tip: Having the fluid taken out of your hip bursa may be momentarily painful. If they don’t offer, ask your doctor for a local anesthetic to numb the area before they take the sample.
Treating Hip Bursitis
-
1Rest and avoid any activities that irritate your hip until you have recovered. Your best course of action if you’ve been diagnosed with bursitis is to rest for at least 1 week, or longer if your symptoms continue. Don’t try to do anything physically challenging. You may even want to take a few days off from work if you have a physically demanding job.[14]
- Check with your doctor if you are unsure about when you can resume your normal activities.
-
2Use NSAID pain relievers to help control pain and inflammation. You can take an over-the-counter pain reliever, such as ibuprofen to help relieve the pain and inflammation in your hip. Follow the manufacturer’s instructions for dosing or ask your doctor for a recommendation.[15]
- If the pain is severe, your doctor may give you a prescription pain reliever instead, such as a high dose ibuprofen or an opioid pain reliever. Take these exactly as your doctor directs you to.
-
3Take antibiotics if the bursitis is caused by an infection. Follow your doctor’s instructions for how to take the antibiotics. Some antibiotics can be taken with food while others need to be taken on an empty stomach, so check the instructions to be sure. Complete the entire course of antibiotics as well. Do not stop taking them until they are all gone, even if you feel better.[16]
-
4Get a steroid injection to relieve pain for 2 months or longer. If your bursitis is severe or chronic and an infection has been ruled out, your doctor may recommend getting a steroid injection to help with the pain. This will reduce the inflammation in your bursa as well. Your doctor can administer the steroid shot in their office and it only takes a few minutes to start working.[17]
- The effects of a steroid shot can last for 2 months or longer so this may be a good option if bursitis is an ongoing problem for you.
Warning: Using steroid injections to control bursitis pain is not a long-term solution as it can eventually cause damage to the surrounding tissues. Steroid injections also pose a high risk of complications if the person’s bursa fluid is infected, so they are not recommended in these situations.
-
5Walk with a cane or crutches to take the pressure off your hip. An assistive device, such as a cane, crutches, or even a walker can be a helpful way to let your hip rest while you go about your daily activities. Use the device to reduce the pressure on your hips when you walk by leaning into it and supporting yourself with your upper body.[18]
- Ask your doctor to demonstrate the proper way to use a walker if you are unsure.
-
6See a physical therapist to learn about exercises and stretches. Another way to help with chronic bursitis is to address the root cause, which may require strengthening and stretching the muscles around your hip. A physical therapist can show you safe ways to do this such as by guiding you through a tailored routine.[19]
- Ask your doctor for a referral to a physical therapist if you’re interested in learning an exercise and stretching routine that may help to ease your hip pain and prevent it from recurring.
-
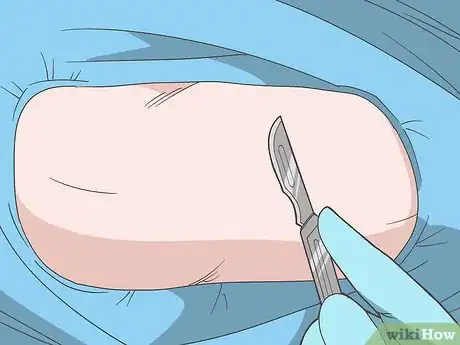
7Discuss surgical removal of the bursa for chronic hip bursitis. In severe cases of chronic bursitis, a surgical procedure to remove the bursa may be the best option for treating the condition and preventing it from coming back. Discuss this option with your doctor along with all of the potential risks and benefits of this surgery.[20]
- Keep in mind that this is usually a last resort if other treatment options have failed.
References
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242
- ↑ https://my.clevelandclinic.org/health/diseases/4964-trochanteric-bursitis
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242
- ↑ https://my.clevelandclinic.org/health/diseases/4964-trochanteric-bursitis
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/diagnosis-treatment/drc-20353247
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/diagnosis-treatment/drc-20353247
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://www.mayoclinic.org/diseases-conditions/bursitis/diagnosis-treatment/drc-20353247
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis
- ↑ https://orthoinfo.aaos.org/en/diseases--conditions/hip-bursitis


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...