This article was co-authored by Jeremy Bartz, PhD. Dr. Jeremy Bartz is a Clinical Psychologist in private practice based in Los Angeles, California. Dr. Bartz specializes in treating depression, anxiety, OCD, mind-body syndromes, chronic pain, insomnia, relationship difficulties, attachment trauma, and resolving the effects of narcissistic trauma. He received a Ph.D. in Counseling Psychology from Brigham Young University and completed a fellowship In Pain Psychology at Stanford's premier pain management clinic.
There are 13 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 48 testimonials and 100% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 1,163,211 times.
Chronic pain is a condition that lasts for three months or more and continues after the injury or condition is treated. The experience of acute pain is the nervous system’s natural response to possible injury. With chronic pain, however, pain signals continue abnormally.[1] This can be both distressing and exhausting for chronic pain sufferers. In some cases of chronic pain, there was an injury, illness or infection that first caused the pain. In other people, though, chronic pain appears and continues without a history of these events. To understand chronic pain sufferers, you should learn about chronic pain, be supportive and know what to say and what not to.
Steps
Learning about Chronic Pain
-
1Find out more about the sufferer’s pain. Each chronic pain sufferer’s experience is unique. It may be helpful if they talk about the condition and their daily battle with pain. The more you know about what the chronic pain sufferer is going through, the more you will be able to understand what it’s like for them.[2]
- Did they suffer from a sprained back, serious infection or is there an ongoing cause of pain such as arthritis, diabetic neuropathy, or some other form of nerve damage? Know when the pain started, and do some research or read stories about people with similar issues.
- Sometimes doctors cannot find the source of the pain, but are aware that the patient is suffering from the pain on a daily basis.
- Don’t push a chronic pain sufferer to talk about things they don’t want to. For some people, bringing it up will just make them feel worse.
- Common chronic pain complaints include headache, low back pain, arthritis pain, pain from damage to the peripheral nerves or the central nervous system or pain without any known source.
- A person can have more than one co-existing chronic pain condition, such as chronic fatigue syndrome, endometriosis, sciatica, peripheral neuropathy, or inflammatory bowel disease, or depression.
- Accept that words may be inadequate to describe how the sufferer is feeling. Recall a time when you experienced a lot of pain and imagine that pain being present twenty-four hours a day every day without relief for the rest of your life. It's hard to find the words for that sort of pain.
-
2Learn the code. A numeric pain scale is used to measure pain intensity so healthcare providers can check treatment efficacy. A scale from 1 to 10 describes the pain level. 1 is "no pain at all, feel wonderful" and 10 is the "worst pain ever felt." Ask where they are at on the pain scale.[3]
- Do not assume the chronic pain sufferer is not experiencing pain if they say they are fine. Many sufferers attempt to hide the pain due to a lack of understanding in others.
- When asked about their pain level, chronic pain sufferers may not give you their actual level of pain. Because their pain is chronic, they are used to a certain level of pain and may just accept that as normal or no pain. They may only give you a correct pain level when they have some form of acute pain, when the "normal" level of pain that they live with daily changes, when they experience pain that now feels differently (I.e., "shooting" instead of "aching", " burning" instead of throbbing"), or when they are asked directly about their current levels of both acute and chronic pain.
Advertisement -
3Recognize coping skills. When you have the flu, you probably feel miserable for a few days or weeks but do the best you can to function. Chronic pain sufferers have probably been feeling awful for a long time. They may have adopted coping mechanisms that conceal the real level of pain they feel or they may not have the strength to function normally.[4]
-
4Be aware of depression symptoms. Chronic pain may cause secondary depression (wouldn't you get depressed and down if you were hurting constantly for months or years?). Depression may be due directly to chronic pain, and chronic pain may be directly due to depression.[5]
- Depression can cause some people to show less emotion, which can mask the pain because the sufferer ceases to make it known. Always be on the lookout for signs of depression and do not confuse this with there being any less pain.
- Depression may also cause people to show more emotion (crying and tearful, anxious, irritable, sad, lonely, hopelessness, fear of the future, easily agitated, angry, frustrated, hyper/over talkative due to medications/need to vent/lack of sleep). This, like their pain level, can vary day to day, hour to hour, minute to minute.
- One of the worst things you can do is abandon someone with chronic pain. That just gives them one more reason to be depressed, feel lonely and not be very positive. Try to be there for them and show them support however you can.
-
5Respect physical limitations. With many diseases, a person will exhibit obvious signs of conditions, such as paralysis fever or broken bones. With chronic pain, however, there is no way to tell what a person’s ability to cope with movement is like at any given moment. You can't always read it on their face or in their body language either.[6]
- The sufferer may not know, from day-to-day, how they are going to feel when they wake up. Each day has to be taken as it comes. This can be confusing for everyone but is very frustrating for the sufferer.
- Being able to stand up for ten minutes doesn't mean that the sufferer can stand up for twenty minutes, or an hour. Just because the person managed to stand up for thirty minutes yesterday doesn't imply that they will be able to do the same today.
- Movement is not the only limitation that chronic pain sufferers may experience. One’s ability to sit, walk, concentrate and be sociable can also be affected.
- Be very understanding if the chronic pain sufferer says they have to sit down, lie down, stay in bed or take these pills right now. It probably means that they have no choice and can't put it off just because they happen to be somewhere or are in the middle of doing something. Chronic pain does not wait for anyone.
-
6Look for signs of pain. Grimacing, restlessness, irritability, mood swings, wringing of hands, moaning, sleep disturbance, teeth grinding, poor concentration, decreased activity and perhaps even writing down suicidal thoughts or language can indicate distress or pain. Be sensitive to what they are going through.
-
7Know that chronic pain is real. You might think that chronic pain sufferers go to doctors because they seek attention, enjoy it or are hypochondriacs. What they are actually doing is looking for something to improve the quality of their life, and often they are looking for the cause of their pain if it is not known. No one wants to feel the way they do but they don’t have a choice.[7]
-
8Recognize what you can’t know. Pain is a difficult thing to describe to another person. It is felt personally and is based in both psychological and physical parts of us. Even if you are very empathetic, never assume that you know exactly how it feels for that person. Sure, you know how it feels for you but each of us is different, and it's impossible to get inside a person's skin and feel their pain.
Being Supportive
-
1Practice empathy. Being empathetic means you attempt to understand another person’s feelings, perspectives and behavior by seeing the world through their eyes. You use this understanding to guide what you do for and say to that person. People with chronic pain are different than you in some ways but are also very much like you, so focus on what you have in common and try to understand the differences.[8]
- Being sick does not mean that the sufferer is no longer a human being. Though chronic pain sufferers spend the majority of their day in considerable pain, they still want the same things that healthy people want. They too want to enjoy work, family, friends and leisure activities.
- The chronic pain sufferer may feel as if they are stuck inside a body in which they have little or no control. Pain puts everything you used to enjoy out of reach and can contribute to feelings of helplessness, sadness and depression.
- Try to remember how lucky you are to be physically able to do all of the things that you can do. Then imagine if you couldn’t.
-
2Respect that the person in pain is trying their best. They may attempt to cope, sound happy and look normal as often as they can. They live their lives to the best of their ability. Keep in mind that when the chronic pain sufferer says they are in pain - they are!
-
3Listen. One of the best things that you can do for a chronic pain sufferer is to listen to them. To be a good listener, pay attention and try to understand what is going on inside of that person so that you can grasp how they are feeling and what they really need.[9]
- Make it clear that you want to hear what they have to say. Many people with chronic pain feel that others won’t believe them or will ridicule them for being weak.
- Try to decode what they're hiding or minimizing through body language and tone of voice.
- Allow yourself to be vulnerable. Sharing means you both give something. To create a strong empathetic bond and really make your exchange matter, you will need to reveal your true feelings, beliefs and experiences as well.
- Read How to be a good listener for more details on being a great listener.
-
4Be patient. If you find yourself being impatient and wanting the sufferer to "just get on with it", you risk laying a guilt trip on the person who is suffering from pain and undermining their determination to cope. They probably want to comply with your requests to do things but don’t have the strength or coping capacity as a result of the pain.
- Don't be put off if the chronic pain sufferer seems touchy. They have been going through a lot. Chronic pain wreaks havoc on the body and the mind. These people do their best to cope with how exhausting and exasperating the pain is but can’t always be ok. Try to accept them as they are.
- A chronic pain sufferer may need to cancel a previous commitment at the last minute. If this happens, please do not take it personally.
-
5Be helpful. The chronic pain sufferer depends a great deal on people who are not sick to support them at home or visit them when they're too sick to go out. Sometimes they need help with bathing, dressing, personal cares, etc. They may need help getting to the doctor. You can be their link to the "normality" of life and help them keep in touch with the parts of life that they miss and desperately want to undertake again.[10]
- Many people offer to help but really aren't there when asked to be. If you offer to help, make sure you follow through. The person with chronic pain that you care about is depending on you.
-
6Balance your caregiving responsibilities. If you are living with a chronic pain sufferer or supporting such a person on a regular basis, you need to maintain balance in your own life. If you don't take care of your own needs, health and work-life balance, being around the chronic pain sufferer can really bring you down. Avoid suffering from carer burn-out by getting other people to help and taking time out. Care for this person as much as you're able but remember to also care for yourself.[11]
-
7Treat them with dignity. Although the person with chronic pain has changed, they think the same. Remember who they are and the things they did before the pain became so bad. They are still the intelligent mind that made a good living at a job they may have loved and had no choice but to give up. Be kind, thoughtful and don’t patronize them.[12]
- Punishing an ill person for not following through with something will make them feel worse and show them that you really don't understand. Those experiencing chronic pain already deal with more than most could ever comprehend. Try to understand why they couldn’t follow through.
-
8Include them in your life. Just because someone cannot do certain activities very often or has cancelled before does not mean that you shouldn't ask them to join you or should hide that you have plans from them. There may be some days when that activity is manageable, and chronic pain is isolating enough! Please understand and keep asking.[13]
-
9Offer a hug. Instead of suggesting how sufferers can fix their pain, consider being empathetic and giving them a gentle hug to let them know you're there to support them. They already hear and see endless doctors who tell them how to fix or help their chronic pain.
- Sometimes just laying your hand on the shoulder of someone can help give them comfort. A hug can be incredibly comforting to someone in pain, especially when no solution is in their sight. You may need to ask first. “Can I give you a hug?” is a good place to start. For some people, touch can be painful, so asking them gives them the chance to tell you yes or no, and if they need special care such as a hug with firm or light pressure, no rubbing, or avoidance of certain painful areas. Remember to be gentle. A hug can build a connection and let them know you’re there to support them.
Knowing What to Say
-
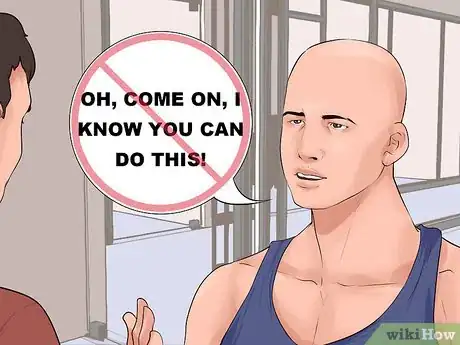
1Leave your pep talk for your kids and gym buddies. Realize that chronic pain is variable and a pep talk can be aggravating and demoralizing for the chronic pain sufferer. If you want them to do something, then ask if they can and respect their answer.
- Try not to say: "But you did it before!" or "Oh, come on, I know you can do this!"
- Staying as active as possible and partaking in activities like walking, biking, and tai chi may help ease muscle and joint pain. Sometimes being sedentary causes pain to get worse. However, don’t lecture on the value of exercise and fresh air. For a chronic pain sufferer, these things may not help the pain and can often exacerbate it. Telling them that they need to exercise or do something to "get their mind off of it" may frustrate them. If they were capable of doing these things any or all of the time, they would.
- Another statement that hurts is, "You just need to push yourself more, try harder". Sometimes participating in a single activity for a short or long period of time can cause more damage and physical pain for the chronic pain sufferer—not to mention the recovery time, which can be intense.
- An individual with chronic pain does not need to be told "You are too sensitive", "You have to deal with it better" or "You have to do it for X, Y or Z". Of course they are sensitive! You have no idea what they cope with or the amount of pain or worry they deal with.
-
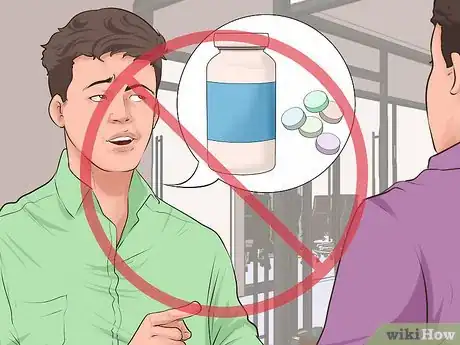
2Don’t play doctor. Chronic pain sufferers are constantly working with doctors, striving to improve and do the right things for their illness. You may not give the correct advice, especially if you're not medically trained and haven't got a clue what that person is dealing with.[14]
- Be sensitive when suggesting medicines or alternative treatments. Prescription drugs, over-the-counter medicines and alternative therapies can have side effects and unintended consequences.
- Some sufferers may not appreciate suggestions—but it's not because they don't want to get well. They may have heard of it or tried it already. They may not be ready to cope with a new treatment that can create an additional burden on their already over-burdened lives. Treatments that haven't worked carry the emotional pain of failure, which in and of itself can make the person feel worse.
- If there is something that cured or helped people with a particular form of chronic pain like theirs, then let the sufferer know when they seem receptive and are ready to hear it. Be sensitive to how you bring it up.
- Don't lecture about prescription medicine if they've been prescribed by a doctor. Pain control is hard to manage and some days these sufferers may require more pain medicine than others. Tolerance is NOT addiction.
- Avoid being judgmental about drug use pursued by chronic pain sufferers.
-
3Never use throwaway lines. Don’t assume you know best by making statements such as "Ah well, that's life, you'll just have to deal with it", or "You'll get over it eventually”, “Until then, you'll just have to do your best", or worst of all, "Well, you look well enough", etc. These lines are a form of distancing yourself from the ill person. Often, it just makes the sufferer feel worse and out of hope.[15]
- People who live with chronic pain know how they feel and are well aware of their situation, so avoid projecting onto the sufferer how you think they should be feeling.
- Throw lifelines rather than throwaway lines by saying something like: "So how can I help you", or "is there anything that I can do to help you deal with your pain?"[16]
-
4Don't compare health problems. Don't say “I've had that before and I'm fine now”. It shows your lack of understanding and makes the person living with chronic pain feel like a failure that they can't handle what they are experiencing and others would do a much better job in the same situation.
-
5Be positive. It's awful living with chronic pain, but it's even worse when people give up on them, misunderstand them or spread negativity. Everyday life can be hard and very lonely for chronic pain sufferers. Constant support, offering hope and showing your love are all crucial things to communicate to them.
- Comfort those with chronic pain, and let them know that you are there for them. A loyal friend is a life saver!
-
6Ask about their treatment. Inquire how satisfied the sufferer is with their treatment. It’s important to ask helpful questions about whether the chronic sufferer thinks their treatment is satisfactory or if they think their pain is bearable. People rarely ask these open-ended "helpful questions" that might help the chronic sufferer open up and really talk.
-
7Ask how they are. Don't stop asking someone with chronic pain "How are you?" just because the answer might be uncomfortable for you. It may be the only opportunity to show you care about their well-being. And if you don't like the answer, remember that it is their answer—not your opinion.
- When the ill person finally opens up to someone, they should not be told that they "talk about it too much" or it's "all they talk about". Recognize that pain is probably a huge part of their lives. They may not want to talk about things like vacations, shopping, sports or gossip.
-
8Know that silence is ok too. Sometimes sharing silence together is good, and the sufferer is just happy to have you there with them. You don't have to fill every minute of conversation with words. Your presence says a whole lot!
-
9Admit when you don't have answers. Don't use platitudes or bold allegations not based on fact to hide your ignorance. There is much even the medical community does not know about chronic pain. There is no harm in saying "I don't know" and then offering to find things out.[17]
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionWhat even is chronic pain?
 David Schechter, MDDr. David Schechter is a physician in Culver City, California. With over 25 years of experience as a family and sports medicine physician, Dr. Schechter specializes in mind-body medicine, preventive medicine, and chronic pain. Dr. Schechter received his MD from New York University and is an attending physician at Cedars-Sinai Medical Center. He was named a Top Doctor by Los Angeles Magazine and Men's Health Magazine. He has also written several books, including The MindBody Workbook.
David Schechter, MDDr. David Schechter is a physician in Culver City, California. With over 25 years of experience as a family and sports medicine physician, Dr. Schechter specializes in mind-body medicine, preventive medicine, and chronic pain. Dr. Schechter received his MD from New York University and is an attending physician at Cedars-Sinai Medical Center. He was named a Top Doctor by Los Angeles Magazine and Men's Health Magazine. He has also written several books, including The MindBody Workbook.
Family Medicine Practitioner
-
QuestionShould people with chronic pain avoid being active? Will that make their pain worse?
 Jeremy Bartz, PhDDr. Jeremy Bartz is a Clinical Psychologist in private practice based in Los Angeles, California. Dr. Bartz specializes in treating depression, anxiety, OCD, mind-body syndromes, chronic pain, insomnia, relationship difficulties, attachment trauma, and resolving the effects of narcissistic trauma. He received a Ph.D. in Counseling Psychology from Brigham Young University and completed a fellowship In Pain Psychology at Stanford's premier pain management clinic.
Jeremy Bartz, PhDDr. Jeremy Bartz is a Clinical Psychologist in private practice based in Los Angeles, California. Dr. Bartz specializes in treating depression, anxiety, OCD, mind-body syndromes, chronic pain, insomnia, relationship difficulties, attachment trauma, and resolving the effects of narcissistic trauma. He received a Ph.D. in Counseling Psychology from Brigham Young University and completed a fellowship In Pain Psychology at Stanford's premier pain management clinic.
Clinical Psychologist Actually, patients with chronic pain should try to be as active as is deemed allowable by their physician. There are probably only a limited number of things that are truly off-limits because they could worsen their condition, but they should do other activities (remembering to pace themselves to avoid pain flares). They can come up with a protocol with a skilled pain psychologist.
Actually, patients with chronic pain should try to be as active as is deemed allowable by their physician. There are probably only a limited number of things that are truly off-limits because they could worsen their condition, but they should do other activities (remembering to pace themselves to avoid pain flares). They can come up with a protocol with a skilled pain psychologist. -
QuestionAre opioids good for chronic pain?
 Jeremy Bartz, PhDDr. Jeremy Bartz is a Clinical Psychologist in private practice based in Los Angeles, California. Dr. Bartz specializes in treating depression, anxiety, OCD, mind-body syndromes, chronic pain, insomnia, relationship difficulties, attachment trauma, and resolving the effects of narcissistic trauma. He received a Ph.D. in Counseling Psychology from Brigham Young University and completed a fellowship In Pain Psychology at Stanford's premier pain management clinic.
Jeremy Bartz, PhDDr. Jeremy Bartz is a Clinical Psychologist in private practice based in Los Angeles, California. Dr. Bartz specializes in treating depression, anxiety, OCD, mind-body syndromes, chronic pain, insomnia, relationship difficulties, attachment trauma, and resolving the effects of narcissistic trauma. He received a Ph.D. in Counseling Psychology from Brigham Young University and completed a fellowship In Pain Psychology at Stanford's premier pain management clinic.
Clinical Psychologist
References
- ↑ David Schechter, MD. Family Medicine Practitioner. Expert Interview. 15 July 2020.
- ↑ David Schechter, MD. Family Medicine Practitioner. Expert Interview. 15 July 2020.
- ↑ https://specialistshospitalshreveport.com/patient-resources/using-the-pain-scale/
- ↑ https://www.apa.org/topics/pain/chronic
- ↑ https://www.journalslibrary.nihr.ac.uk/pgfar/pgfar04140/#/abstract
- ↑ https://pubmed.ncbi.nlm.nih.gov/23126682/
- ↑ https://www.theguardian.com/australia-news/2021/jun/28/sufferers-of-chronic-pain-have-long-been-told-its-all-in-their-head-we-now-know-thats-wrong
- ↑ http://greatergood.berkeley.edu/article/item/six_habits_of_highly_empathic_people1
- ↑ https://www.health.qld.gov.au/news-events/news/caring-for-someone-with-chronic-pain
- ↑ https://www.health.qld.gov.au/news-events/news/caring-for-someone-with-chronic-pain
- ↑ https://journals.sagepub.com/doi/full/10.1177/2158244013512130
- ↑ https://www.northernpaincentre.com.au/wellness/chronic-pain-relationships/chronic-pain-and-relationships/
- ↑ https://www.northernpaincentre.com.au/wellness/chronic-pain-relationships/chronic-pain-and-relationships/
- ↑ https://www.abc.net.au/everyday/things-not-to-say-to-a-person-living-with-chronic-pain/12338488
- ↑ https://www.abc.net.au/everyday/things-not-to-say-to-a-person-living-with-chronic-pain/12338488
- ↑ https://www.psychologytoday.com/us/blog/turning-straw-gold/201207/what-those-chronic-pain-or-illness-do-want-hear
- ↑ https://www.va.gov/WHOLEHEALTHLIBRARY/tools/communicating-about-chronic-pain-instructions-for-clinicians.asp
About This Article
To understand someone with chronic pain, ask them where the pain they're feeling falls on the pain scale from 1 to 10, where 1 is no pain at all and 10 is the worst pain they've ever felt. You can also keep an eye out for common signs of pain, like grimacing, irritability, and moaning, so you know when they're hurting. While you can't actually feel the pain they're experiencing, you can try asking them about what they're going through so you understand it more. To learn how to be supportive of someone with chronic pain, scroll down.


























-with-Jaw-Exercises-Step-11.webp)
-Step-20-Version-2.webp)















-with-Jaw-Exercises-Step-11.webp)
-Step-20-Version-2.webp)




































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...