This article was co-authored by Dale Prokupek, MD. Dale Prokupek, MD is a board-certified Internist and Gastroenterologist who runs a private practice based in Los Angeles, California. Dr. Prokupek is also a staff physician at Cedars-Sinai Medical Center and an associate clinical professor of medicine at the Geffen School of Medicine at the University of California, Los Angeles (UCLA). Dr. Prokupek has over 30 years of medical experience and specializes in the diagnosis and treatment of diseases of the liver, stomach, and colon, including chronic hepatitis C, colon cancer, hemorrhoids, anal condyloma, and digestive diseases related to chronic immune deficiency. He holds a BS in Zoology from the University of Wisconsin – Madison and an MD from the Medical College of Wisconsin. He completed an internal medicine residency at Cedars-Sinai Medical Center and a gastroenterology fellowship at the UCLA Geffen School of Medicine.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 20,967 times.
Inflammatory bowel disease (IBD) is a catchall phrase that includes several diseases that cause inflammation in your digestive system. The main diseases included under this umbrella are Crohn's disease and ulcerative colitis.[1] If you are having a flare-up, a liquid diet may be helpful in reducing inflammation so you can go back to regular food. Any change in diet, particularly when you have a disease that affects the absorption of nutrients like IBD, should be approved by your doctor.
Steps
Deciding If You Need a Liquid Diet
-
1Use a liquid diet for severe inflammation. A liquid diet is often prescribed by a doctor if you have severe inflammation. Usually, patients who go on this diet are waiting to have surgery done on their bowels to improve their situation, and the liquid diet is a temporary solution until surgery can happen. It is sometimes used after surgery, as well.
- You may also try a partially liquid diet during a flare-up.
- Often, this diet is only used for about two to eight weeks at a time, depending on the type of diet.[2]
- However, some people do need to use it for much longer. For instance, some people use it for a year or longer, though it may also cause you to lose weight.[3]
-
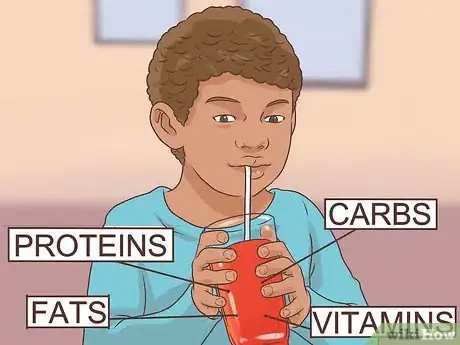
2Take liquid nutrition for better absorption. People with IBD are often at risk of malnutrition and nutritional deficiencies, particularly if they have Crohn's Disease or ulcerative colitis. A liquid diet can help you better absorb the nutrients your body needs. The liquid is composed of the base components of nutrition, including proteins, fats, carbohydrates, and vitamins, making it easier for those with IBD to absorb. Often, the proteins are broken down into component parts, which means your stomach has to work less to digest it.
- Think about it this way: normally, your mouth and stomach begin the process of breaking down large pieces of food. In the case of a liquid diet, it doesn't need to be broken down into smaller pieces because it's already liquid. In fact, sometimes this diet is used to skip the stomach altogether, through the use of a tube.
- Children, especially, benefit from this treatment, as it ensures they get adequate nutrition even if they have a poor appetite.[4]
- If you think you are at risk for malnutrition, speak with your doctor or nutritionist.
Advertisement -
3Try the diet in place of corticosteroids. Often, this diet is used in place of corticosteroids as a treatment. If you have sensitivity to these medications, for instance, this diet may be a better option. It can help control inflammation, though it may not put you in full remission.[5]
-
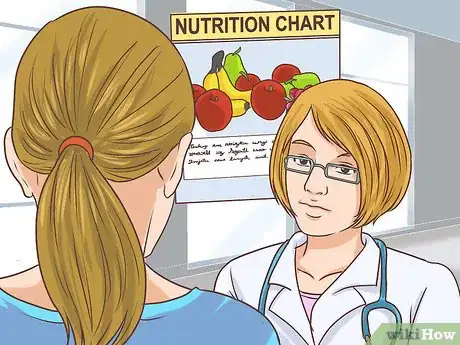
4Talk to your doctor. Before making a drastic diet change like going to a liquid diet, it's always best to discuss it with your doctor first. With IBD, your ability to absorb nutrients is reduced, and going to a liquid diet is a big change that many people have difficulty sticking to.[8]
- When talking with your doctor, bring up why you think a liquid diet would be a good option for you. You could try, "I've been having almost continuous flare-ups lately, and I was wondering if a liquid diet may help reduce those occurrences, at least in the short-term."
- If you're having flare-ups, your doctor can put you in contact with a nutritionist that may be able to help you tailor your diet to reduce flare-ups.
Using a Prescribed Liquid Diet
-
1Discuss which liquid diet is most appropriate for you. Three types of liquids are used for this diet: elemental, semi-elemental, and polymeric. Elemental diets contain just amino acids (the building blocks of protein), while polymeric contain whole protein strands. Semi-elemental are somewhere in the middle. That means that elemental diets are the easiest to digest, but they also taste the worst of the three.[9]
- Ask your doctor which would be the best option for you.
-
2Purchase an appropriate drink. Once you've narrowed down what kind of liquid diet you need, your doctor can recommend an appropriate brand. You can find these drinks at most drug stores and big box stores, so they are readily available.[10]
- Some elemental brands include Vivonex, Tolerex, and Alitraq.
- Some semi-elemental brands include Peptamen or Peptamen Junior, Optimental, Subdue, Perative, and Vital HN.
- A few polymeric brands are Promote, Probalance, Replete, Jevity, and Isocal.[11]
-
3Be ready for some discomfort. You can take these diets by mouth; however, they are not the most tasty drinks. Polymeric tends to taste somewhat better than elemental diets. Nonetheless, you may find the drink unpleasant.[12]
- You can take the diet through other methods. For instance, you can take it through a tube in your nose at night, though some people find it uncomfortable.[13] In some cases, this type of diet may be taken through a tube that goes directly to the intestine or stomach.
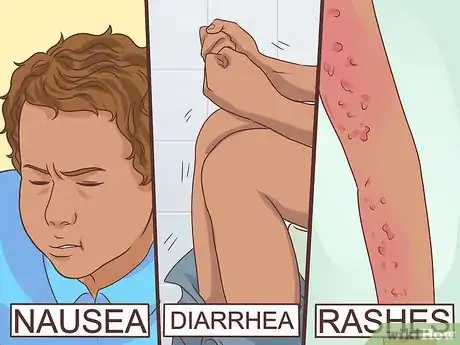
- You may also experience other problems with this diet, such as nausea or diarrhea. A few people report skin rashes while on this type of diet, but those generally clear up. Also, in patients with diabetes, the diet may contain too much sugar, and insulin may need to be adjusted.[14]
-
4Stay exclusively on the prescribed diet. For this diet to work well, you must exclude all other foods and liquids, with the exception of water. You'll be getting your nutrition solely from the liquid to give your bowels a chance to heal from the inflammation.[15]
- In some cases, your doctor may prescribe these liquids as a supplement to your normal diet. Either way, the key is to stay on the diet as prescribed by your doctor or nutritionist.
-
5Try parenteral nutrition for severe cases. Sometimes, you may not even be able to use your digestive system to absorb nutrients. In that case, you can take nutrients right into your bloodstream, using an IV catheter. The mixture is still made up of the same base components; it just goes into your blood rather than into your digestive system.
- This method allows your bowels to be rested completely.
Returning to Regular Food
-
1Try diluted juices. One way to get some nutrients after a flare up is to drink juices that have been watered down a bit. Watered down is best because too much sugar can also cause irritation. However, the juices will provide you with some of the nutrients you need.[16]
- Low-sugar sports drinks can also be beneficial.
-
2Skip the ice. Although you may enjoy your drinks ice-cold, you may have better luck trying warmer beverages, such as room temperature. Ice-cold liquids can cause you to have cramps, making symptoms worse and causing you more pain.
-
3Avoid caffeine. If possible, skip the caffeine altogether. Caffeine doesn't just boost your energy, it also gives a "boost" to your bowels. In other words, it can lead to diarrhea in people who already have bowel trouble, so it's best to avoid it.
-
4Slow down. While you want to get plenty of fluids on a liquid diet, try not to gulp your beverages down. Instead, go a bit more slowly and avoid using a straw. Going too fast or using a straw introduces more air into your system, which can lead to you having extra gas and being uncomfortable.
-
5Move up to solids. Once your doctor says it's okay, you can start slowly introducing solids, beginning with soft foods. Try adding one new food a day, so you don't overwhelm your system. You can begin with foods like applesauce and oatmeal. [17]
- Other well-tolerated solids include plain poultry or fish, eggs, plain mashed potatoes, plain noodles, bread (white or sourdough), and canned fruits.
- If you have Crohn's disease, ulcerative colitis, or are on a low-residue/low-roughage diet, be wary of oatmeal, as it is roughage and contains a lot of fiber.
Expert Q&A
-
QuestionHow much fiber should I eat if I'm trying to cleanse my colon?
 Dale Prokupek, MDDale Prokupek, MD is a board-certified Internist and Gastroenterologist who runs a private practice based in Los Angeles, California. Dr. Prokupek is also a staff physician at Cedars-Sinai Medical Center and an associate clinical professor of medicine at the Geffen School of Medicine at the University of California, Los Angeles (UCLA). Dr. Prokupek has over 30 years of medical experience and specializes in the diagnosis and treatment of diseases of the liver, stomach, and colon, including chronic hepatitis C, colon cancer, hemorrhoids, anal condyloma, and digestive diseases related to chronic immune deficiency. He holds a BS in Zoology from the University of Wisconsin – Madison and an MD from the Medical College of Wisconsin. He completed an internal medicine residency at Cedars-Sinai Medical Center and a gastroenterology fellowship at the UCLA Geffen School of Medicine.
Dale Prokupek, MDDale Prokupek, MD is a board-certified Internist and Gastroenterologist who runs a private practice based in Los Angeles, California. Dr. Prokupek is also a staff physician at Cedars-Sinai Medical Center and an associate clinical professor of medicine at the Geffen School of Medicine at the University of California, Los Angeles (UCLA). Dr. Prokupek has over 30 years of medical experience and specializes in the diagnosis and treatment of diseases of the liver, stomach, and colon, including chronic hepatitis C, colon cancer, hemorrhoids, anal condyloma, and digestive diseases related to chronic immune deficiency. He holds a BS in Zoology from the University of Wisconsin – Madison and an MD from the Medical College of Wisconsin. He completed an internal medicine residency at Cedars-Sinai Medical Center and a gastroenterology fellowship at the UCLA Geffen School of Medicine.
Board Certified Internist & Gastroenterologist You want to get between 25-30 grams of fiber every single day if you're cleansing your colon. If you can't get enough fiber from your diet, you can take a supplement. As a note, this is basically the only way to efficiently cleanse your colon. Other options are just not going to be as effective.
You want to get between 25-30 grams of fiber every single day if you're cleansing your colon. If you can't get enough fiber from your diet, you can take a supplement. As a note, this is basically the only way to efficiently cleanse your colon. Other options are just not going to be as effective.
References
- ↑ https://www.cdc.gov/ibd/what-is-IBD.htm
- ↑ http://www.crohns.org.uk/crohns_disease/nutritional_therapy/which-dietary-treatment-should-i-choose
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/54639
- ↑ http://www.crohnscolitisfoundation.org/assets/pdfs/diet-nutrition-2013.pdf
- ↑ http://www.crohns.org.uk/crohns_disease/nutritional_therapy/which-dietary-treatment-should-i-choose
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1378738/pdf/gut00604-0063.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1410941/pdf/gut00494-0076.pdf
- ↑ Dale Prokupek, MD. Board Certified Internist & Gastroenterologist. Expert Interview. 16 April 2020.
- ↑ http://www.crohns.org.uk/crohns_disease/nutritional_therapy/which-dietary-treatment-should-i-choose
- ↑ https://www.ucsfhealth.org/education/nutrition_tips_for_inflammatory_bowel_disease/
- ↑ https://med.virginia.edu/ginutrition/wp-content/uploads/sites/199/2015/11/MakolaArticle-Dec-05.pdf
- ↑ http://www.crohns.org.uk/crohns_disease/nutritional_therapy/which-dietary-treatment-should-i-choose
- ↑ http://www.med.umich.edu/ibd/education/diet.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1410941/pdf/gut00494-0076.pdf
- ↑ http://www.crohns.org.uk/crohns_disease/nutritional_therapy/which-dietary-treatment-should-i-choose
- ↑ https://www.ucsfhealth.org/education/nutrition_tips_for_inflammatory_bowel_disease/
- ↑ https://www.ucsfhealth.org/education/nutrition_tips_for_inflammatory_bowel_disease/





















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...