This article was written by Roy Nattiv, MD and by wikiHow staff writer, Jennifer Mueller, JD. Dr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 18,435 times.
With laryngopharyngeal reflux (LPR), stomach acid moves up your esophagus into your throat. If you have gastroesophageal reflux disease (GERD), you may develop LPR. The symptoms can include a sore throat, persistent hoarseness, heartburn, and even choking, gagging, or coughing in your sleep.[1]
LPR is common in people who are overstressed, consistently wear clothing that compresses your waist (such as tight pants, belts, or girdles), or struggle with excess weight. LPR is typically treatable through diet. However, more severe cases may require prescription medication or, in rare cases, surgery.[2]
This article is based off an interview with our board certified gastroenterologist, Roy Nattiv, MD. Check out the full interview here.
Steps
Controlling LPR through Diet
-
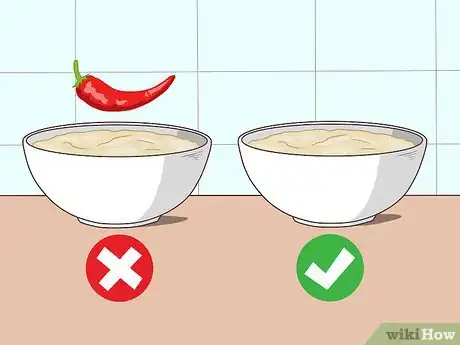
1Choose bland rather than spicy foods. Spicy foods can make heartburn worse, and may also increase reflux symptoms generally.[3] Heavily seasoned and spicy foods encourage your stomach to produce more acid.[4]
- In general, start by eliminating all condiments and seasonings except black pepper. If there are particular condiments or seasonings you like, add them back 1 at a time and monitor your reflux symptoms.
-
2Consume skim or low-fat dairy products. Full-fat dairy products, including milkshakes and regular ice cream, can exacerbate reflux symptoms. Stick to skim milk or try alternative non-dairy products (like soy milk), and look for nonfat or low-fat yogurts and cheeses.
- Experiment with eliminating different dairy products from your diet to find out which ones give you reflux. For example, you may find that ice cream causes problems for you. If so, you might try switching to low-fat frozen yogurt.
Advertisement -
3Avoid highly acidic foods and beverages. Reflux occurs when stomach acid acts in combination with the stomach enzyme pepsin. When you have LPR, it's actually pepsin that gets into your throat and airways. When you eat and drink acidic foods and beverages, it creates an acidic environment in your throat for pepsin to flourish and cause irritation.[5]
- Try to avoid tomato-based foods and peppermint, which can all trigger reflux.[6]
- Colas and other carbonated drinks are even more acidic than citrus fruits. If you must drink carbonated beverages, stick to sugar-free, low-carbonation drinks like Fresca.
- Try to avoid foods with a pH of 5 or lower. When in doubt, do an online search to find out about the pH of foods and drinks you are interested in. You might consult a chart like this one: https://www.clemson.edu/extension/food/food2market/documents/ph_of_common_foods.pdf.
-
4Reduce your daily caloric intake. People who have weight issues are at much greater risk for developing reflux conditions, including LPR. If you are struggling with excess weight, talk to your doctor or a registered dietitian about healthy ways to lose weight.[7]
- Generally, eating smaller portions puts less pressure on your esophageal sphincters, allowing them to keep your stomach acid down.
- High-fat and fried foods also may exacerbate your reflux symptoms. Frozen or restaurant foods often are prepared in oils that may promote reflux as well.
-
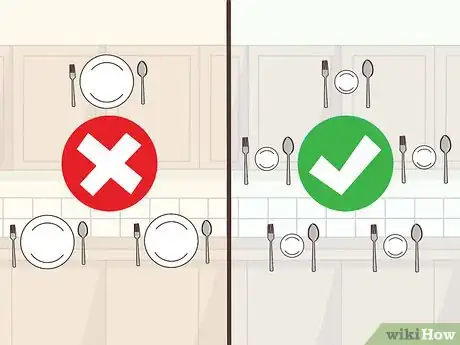
5Eat smaller meals throughout the day. Smaller meals put less pressure on your esophageal sphincters as you digest, making it less likely that you will experience reflux symptoms. Treat your LPR by having 4 or 5 small meals a day, rather than 3 larger ones.[8]
- In addition to eating smaller portions of food, try to eat more slowly. Make sure you thoroughly chew your food before swallowing, and drink water between mouthfuls.
- Allow your food to settle before you engage in any strenuous activities.
-
6Drink plenty of water. Staying well-hydrated can help prevent reflux, and will also keep your throat clear. Aim to drink at least 8 glasses of water a day – more if you're engaging in exercise or other intense physical activity.[9]
- Don't consider other drinks a substitute for water, even if they contain water. For example, although coffee is mostly water, coffee is a diuretic and can trigger reflux.
Eliminating Reflux Triggers
-
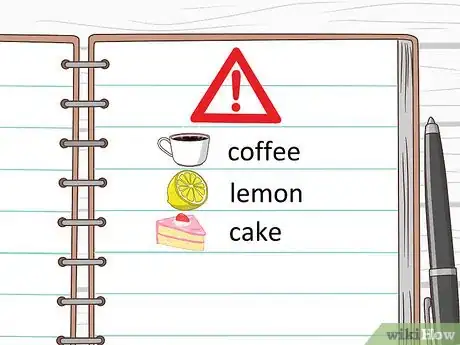
1Keep a food journal to help identify triggers. Specific foods that aggravate reflux differ greatly from person to person. Writing down everything you eat can help you figure out how best to prevent your symptoms.
- There is no universal diet that will successfully treat LPR. Even foods that are common triggers may have no effect on your reflux.
-
2
-
3Quit using tobacco products. Tobacco use, including smoking, dipping, or chewing tobacco, encourages reflux. If you use tobacco, quitting may also resolve your LPR. Ask your doctor for tobacco cessation assistance and resources.[12]
- If you monitor your LPR symptoms immediately after using tobacco, you can see the effect your tobacco use is having on your reflux condition.
-
4Don't eat within 2 hours of going to bed. When you are upright, gravity can assist in keeping your stomach acid down. However, lying down causes the contents of your stomach to press against your lower esophageal sphincter, which can cause reflux.[13]
- In general, avoid eating late at night, when your digestion process is slower. This includes midnight snacks, not just full-blown meals.
-
5Elevate your head when sleeping. Most LPR symptoms happen during the day. However, if you have reflux at night, you may need to put the head of your bed up on blocks to prevent acid from traveling down your throat.[14]
- Propping up on pillows or using a wedge won't work by itself. You have to raise the entire head of the bed 4 to 6 inches (10 to 15 cm).
- Eat at least 2 hours before bedtime to prevent your stomach contents from refluxing when you switch to lying down.[15]
-
6Review all medicines or supplements you're taking. Many over-the-counter and prescription medicines increase the level of acid in your stomach, which can worsen your LPR symptoms. Some nutritional supplements also increase stomach acid.[16]
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) and naproxen (Aleve) can increase stomach acid if you take them regularly and in large doses. If these medications trigger your reflux, try taking half your usual dose. It can also help to take them with a little baby applesauce or caffeine-free tea with milk, so you don’t have an empty stomach.
- Vitamin C supplements also may raise the level of acid in your stomach.
- Blood pressure and asthma medications, as well as birth control pills, may increase stomach acid. If you were prescribed a medication that you believe is worsening your LPR symptoms, talk to your doctor about switching medications. Do not stop taking your medication without first talking to your doctor.
-
7Wear comfortable, loose-fitting clothing. Clothing that constricts your waist can put pressure on your abdomen, making LPR symptoms worse.[17] Avoid tight-fitting jeans, tight belts, or clothes designed to compress your abdomen, such as corsets or body shapers.
- You may find it helpful to switch to pants that have some elastic in the waistband, or that fit lower around your hips instead of high up on your waist.
Seeking Medical Intervention
-
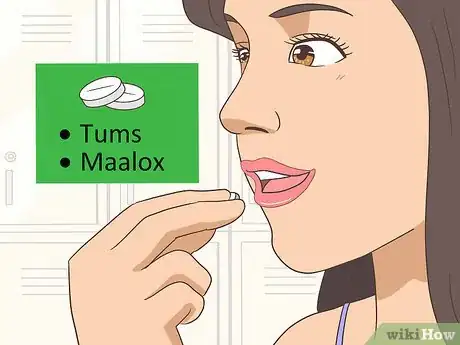
1Try over-the-counter (OTC) medications. Particularly for minor LPR symptoms, OTC antacid medications such as Pepcid, Prilosec, or Tums may provide some short-term relief.[18] These medications are only treating the symptoms, and won't have any effect on the LPR condition itself.[19]
- If you've been diagnosed with LPR, you may want to talk to your doctor even before taking an antacid or other OTC medication. You should also consult your doctor if you find yourself taking an antacid regularly for more than 7 to 10 days in a row.
- Proton-pump inhibitors (PPIs), such as Nexium or Prilosec, are not equally effective for everybody.[20] If these medications don’t seem to be helping your LPR symptoms, talk to your doctor about alternatives.
-
2Discuss prescription medication options with your doctor. If your LPR doesn't improve with changes to your diet, you may want to try a prescription medication that increases the pressure of your weakened sphincters to keep stomach acid down.[21]
- There are also prescription drugs that reduce the number of times the sphincters relax. This can reduce or even eliminate reflux.
- Prescription medications may cause side effects, and some can also interact with other medications you are taking. Talk to your doctor about the risks and benefits of any possible prescriptions, and tell them about other medications you are currently taking.
- These medications can be helpful in the short-term, but if you find yourself needing them for several months, it may be time to discuss surgical options with your doctor.
-
3Consider surgery as a last resort. There are several surgical treatment options for LPR. In most cases, surgical treatment is successful, but it may cause uncomfortable side effects, such as severe bloating.[22]
- Your doctor will be able to discuss surgical options with you, and may refer you to a specialist for further evaluation.
- Keep in mind that surgery typically is a permanent option that cannot be undone, regardless of the side effects you experience as a result.
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionAre there any medications that help with LPR?
 Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Board Certified Gastroenterologist
-
QuestionWhat foods trigger reflux?
 Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Board Certified Gastroenterologist
-
QuestionWhat is LPR?
 Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Board Certified Gastroenterologist
Warnings
- Untreated LPR can cause ulcers in your throat, as well as exacerbating conditions such as bronchitis or emphysema. If changes in your diet and lifestyle do not reduce your LPR, seek medical attention.[23]⧼thumbs_response⧽
References
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ https://my.clevelandclinic.org/health/diseases/15024-laryngopharyngeal-reflux-lpr
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3807765/
- ↑ https://www.refluxgate.com/ultimate-guide-to-lpr-causes-and-treatment
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3807765/
- ↑ https://www.refluxgate.com/ultimate-guide-to-lpr-causes-and-treatment
- ↑ https://patienteducation.osumc.edu/Documents/LPR.pdf
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ https://www.refluxgate.com/ultimate-guide-to-lpr-causes-and-treatment
- ↑ https://www.mwent.com/patient-services/silent-reflux-treatment
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ https://patienteducation.osumc.edu/Documents/LPR.pdf
- ↑ http://www.nyee.edu/patient-care/otolaryngology/voice-swallowing/larynx-disorders/lpr
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 14 October 2020.
- ↑ https://my.clevelandclinic.org/health/diseases/15024-laryngopharyngeal-reflux-lpr/management-and-treatment
- ↑ https://www.refluxgate.com/ultimate-guide-to-lpr-causes-and-treatment
- ↑ https://www.refluxgate.com/ultimate-guide-to-lpr-causes-and-treatment
- ↑ https://www.refluxgate.com/ultimate-guide-to-lpr-causes-and-treatment
- ↑ https://my.clevelandclinic.org/health/diseases/15024-laryngopharyngeal-reflux-lpr/management-and-treatment




































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...