This article was medically reviewed by Luba Lee, FNP-BC, MS and by wikiHow staff writer, Christopher M. Osborne, PhD. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 22,078 times.
Gynecomastia is a condition that causes breast enlargement in males due to glandular growth that’s triggered by a hormonal imbalance. It’s nearly always medically harmless, but it can be damaging to your self-confidence and self-esteem. Get an accurate diagnosis to rule out other possibilities, then work with your doctor to determine the right treatment plan—this can include waiting it out, changing medications and grooming products, attending therapy, and/or undergoing surgery. If you have pseudogynecomastia, which is caused strictly by increased fatty deposits, losing weight through diet and exercise is usually your best option.
Steps
Treating Diagnosed Gynecomastia
-
1See if the condition resolves itself, if possible, if you’re a teen. Gynecomastia is caused by a hormonal imbalance, which is when there are more female hormones (estrogens) than male hormones (androgens). This is why gynecomastia is common among teenage boys going through puberty. In most cases, the condition disappears within a span of about 6 months to 3 years, which means it’s often possible to just “wait it out.”[1]
- Of course, “waiting it out” for a year or two when you’re 15 years old and self-conscious about your body can feel like a lifetime. Do not hesitate to let your doctor know if anxiety or stress about your condition is affecting you. In this case, other treatment options may be warranted.
-
2Avoid soy and other phytoestrogens. Foods that contain soy are phytoestrogens, which means that they may cause your body to make more estrogen. This may cause gynecomastia in some people, so it’s best to avoid soy and other phytoestrogens if you have gynecomastia. Some other foods to limit or avoid include:[2]
- Whole grains
- Dried beans
- Broccoli
- Cauliflower
- Peas
Advertisement -
3Discuss adjusting your meds if they’re a likely cause. Many common medications can cause hormonal imbalances that may contribute to gynecomastia. In some cases, your doctor may be able to switch your meds or adjust your dosage, although this is not always possible. Common medication culprits include:[3]
- Medications to treat an enlarged prostate or prostate cancer.
- Some types of AIDS medications.
- Tricyclic antidepressants.
- Certain types of anti-anxiety medications, such as diazepam.
- Some types of antibiotics.
- Certain antifungal medications, such as ketoconazole.
- Some antacids, such as Tagamet and Zantac.
- Certain blood pressure medications, such as spironolactone.[4]
- Certain heart medications, such as digoxin.
- Gastric motility medications, like metoclopramide.
-
4Take a medication like tamoxifen if you’re on anti-androgen therapy. If you're being treated for prostate cancer or another condition that involves anti-androgen therapy, you may experience gynecomastia as a side effect. In this case, your doctor may prescribe additonal medication to help combat this unwanted side effect.[5]
- In most cases, they'll prescribe an estrogen receptor modulator such as tamoxifen.
- Alternatively, you might be prescribed an aromatase inhibitor like anastrozole.
-
5Switch your body care products if they contain certain plant oils. Lavender oil and tea tree oil in particular contain estrogen-mimicking chemicals, and it’s possible—but not fully proven—that such chemicals may cause gynecomastia. Check your soap, shampoo, body lotion, aftershave, and so on for these oils, and change brands if needed.[6]
- If this is the cause of your gynecomastia, the condition should resolve itself within months after you quit using the products.
- Ask your doctor if there are additional plant oils you should avoid.
-
6Stop using illicit drugs or anabolic steroids, and cut back your alcohol intake. Recreational drugs like marijuana, amphetamines, and heroin can cause hormonal imbalances that may trigger gynecomastia. The same is true for excessive alcohol consumption or the use of anabolic steroids. Work with your doctor to devise the best strategies for quitting.[7]
- Your best option is to quit drinking alcohol altogether, but simply cutting back may result in noticeable improvement.
Warning: Don’t quit a prescribed steroid without your doctor’s approval.
-
7Attend therapy sessions for any related emotional distress. Even though gynecomastia is medically harmless, it can carry a significant emotional toll that you shouldn’t downplay or ignore. If, for example, you feel extremely anxious about taking your shirt off in front of anyone, or have developed low self-esteem due to a negative body image, let your doctor know. They can direct you to a licensed mental health professional.[8]
- Going to therapy sessions may help you to feel more comfortable and confident in your own skin.
- If you develop diagnosed cases of anxiety or depression, your therapist and doctor can develop specific treatment strategies to deal with them.
-
8Choose surgery as a last option and permanent solution. For cases of gynecomastia that are not cured by medication adjustments or other efforts to address hormonal imbalances, there are usually 2 options: living with the condition and hoping it goes away on its own; or, surgery. There are various types of surgery for this condition, depending on the particulars of your situation, but they typically involve the removal of the glandular tissue beneath the areolas.[9]
- In some instances, liposuction will also be performed to remove fatty tissue.
- Nearly all types of surgery for gynecomastia are straightforward and require a limited amount of recovery time. However, like all surgical procedures, they carry risks for problems like infections and blood clots.
- Because gynecomastia is nearly always medically harmless, surgery to address it is typically considered elective, meaning you’ll have to pay out-of-pocket.
Getting a Proper Diagnosis
-
1Tell your doctor if you notice symptoms of gynecomastia. Unlike pseudogynecomastia, which is caused by a buildup of fatty tissue, gynecomastia is specifically caused by an enlargement of glandular tissue due to a hormonal imbalance. Contact your doctor for a checkup if you notice one or more of the following:[10]
- A soft, rubbery lump beneath one or both of your areolas. Contact your doctor right away if you notice any hard lumps, or if you have any type of discharge from one or both nipples. These could be signs of cancer or other conditions.
- Breast enlargement focused around one or both areolas, with or especially without a buildup of soft, fatty tissue in other areas of both breasts.
- Tenderness or soreness when you press on the area around one or both areolas.
Warning: Tell your doctor immediately if you feel outright pain when pressing on the area around your areola.
-
2Share your relevant health history and family history with your doctor. Respond to your doctor’s questions as thoroughly as possible so that they have the information they need to inform their diagnosis. They may ask for information regarding any or all of the following:[11]
- Any other symptoms you may be having.
- Any other medical problems you have had in the past.
- Any history of related health problems in your family.
- What medications, drugs, dietary supplements, or body care products you might be using.
-
3Undergo testing to confirm gynecomastia and/or rule out other causes. Your doctor will likely begin with a physical exam of the area. If they find evidence of gynecomastia, they’ll probably move on to further tests that can both confirm the diagnosis and rule out other potential causes. Such tests can include the following:[12]
- Blood tests, which may include thyroid function, liver function, and kidney function tests. They may also check your luteinizing and follicle-stimulating hormone, free testosterone, and serum estradiol.
- CT scans, an MRI, or a chest X-ray.
- A mammogram.
- A testicular ultrasound, which may detect evidence of a hormonal imbalance.
- A biopsy of your breast tissue, if cancer is suspected.
Managing Pseudogynecomastia
-
1Commit to a healthy weight loss plan using diet and exercise. Because pseudogynecomastia is caused strictly by a buildup of fatty tissue in the breasts, shedding body fat with a sensible weight loss plan is your best option.[13] Talk to your doctor before beginning your weight loss plan—they can help you determine your ideal weight and the best combination of dietary changes and physical activity that can get you there.[14]
- Under your doctor’s guidance, reduce your daily calorie intake; eat more fruits and vegetables, whole grains, lean proteins, and healthy fats; and cut back on packaged and processed foods, high-sodium foods, unhealthy fats, and sugary drinks.
- With your doctor’s approval, aim for 150+ minutes of moderate-intensity aerobic exercise per week, 2-3 strength training sessions per week, and 2-3 flexibility training sessions per week.
Tip: Make an appointment to see an endocrinologist if you’re unable to lose weight with diet and exercise.
-
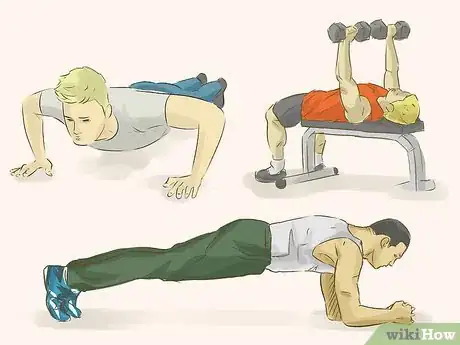
2Use targeted strength training to help sculpt your chest muscles. Despite what you may have heard, you can’t target a specific area—such as your chest—for fat burning. However, you can do targeted strength training exercises to add muscle tone and definition to your chest.[15] This, in combination with overall fat-burning exercises, can help minimize the appearance of pseudogynecomastia.
- Incorporate the following into your routine, for example: push-ups; planks; bench presses; flyes. Consider working with a trainer to make sure you’re doing the exercises correctly.
- Keep in mind that if you build too much muscle in your pecs, they may end up looking even larger than before. Aim for sculpting and definition, not the physique of a “World’s Strongest Man” contestant.
-
3Wear a compression shirt or loose over-shirt, or combine them. Getting rid of pseudogynecomastia takes time, and in some cases it won’t go away completely. If you’re a bit self-conscious about your look, use flattering clothing to flatten and/or conceal your chest area.[16]
- Wear a compression tank-top or T-shirt under your typical shirt to “suck in” your chest. You can even try using a neoprene wrap or other bindings. Always make sure the compression allows for good blood flow and easy breathing, though.
- Try a collared button-down shirt that’s made to be kept untucked, and wear it unbuttoned over a T-shirt (with or without a compression shirt underneath). This combo will help conceal your chest.
-
4Talk to your doctor about additional options. If pseudogynecomastia is causing you a great deal of distress, ask your doctor to recommend a therapist who can help you to feel more confident and comfortable in your own body. You might also discuss options for elective surgery, such as liposuction.[17]
- Surgery for pseudogynecomastia isn’t risk-free, of course, but it is typically a routine procedure with limited risks and recovery time. As an elective procedure, though, you’ll likely have to pay out-of-pocket.
References
- ↑ https://my.clevelandclinic.org/health/diseases/16227-enlarged-male-breast-tissue-gynecomastia
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4270274/
- ↑ https://my.clevelandclinic.org/health/diseases/16227-enlarged-male-breast-tissue-gynecomastia/management-and-treatment
- ↑ https://www.uptodate.com/contents/gynecomastia-breast-enlargement-in-men-beyond-the-basics/print
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3071351/
- ↑ https://www.ncbi.nlm.nih.gov/pubmed?term=17267908
- ↑ https://familydoctor.org/condition/gynecomastia/
- ↑ https://my.clevelandclinic.org/health/diseases/16227-enlarged-male-breast-tissue-gynecomastia/management-and-treatment
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3071351/
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/gynecomastia
- ↑ https://familydoctor.org/condition/gynecomastia/
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/gynecomastia
- ↑ https://www.plasticsurgery.org/news/blog/four-tips-to-prepare-for-gynecomastia-surgery
- ↑ https://familydoctor.org/what-you-should-know-before-you-start-a-weight-loss-plan/
- ↑ https://www.health.harvard.edu/exercise-and-fitness/7-tips-for-a-safe-and-successful-strength-training-program
- ↑ https://www.plasticsurgery.org/news/blog/four-tips-to-prepare-for-gynecomastia-surgery
- ↑ https://www.plasticsurgery.org/news/blog/four-tips-to-prepare-for-gynecomastia-surgery






















-Step-12-Version-2.webp)














































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...