This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 93,790 times.
Contact dermatitis often appears as red, itchy, irritating bumps over dry, cracked, or scaly skin. Your skin may or may not have a burning sensation and, in more severe cases, there may be blisters that ooze and crust over. Contact dermatitis happens in response to your skin being in contact with an irritant or allergen that subsequently triggers an unwanted immune response. In addition to avoiding further contact with the causative agent, there are a variety of at-home treatments and medical treatments that you can try to soothe your symptoms and to speed the healing of your contact dermatitis.
Steps
Trying At-Home Treatments
-
1Identify and avoid the triggering substance. One of the key steps in treating contact dermatitis is to identify the causative agent, and to avoid further exposure to whatever it is that triggered your contact dermatitis in the first place. Symptoms often appear a day or so after exposure to the trigger, and the rash will cover the area of skin that was in direct contact with the triggering agent. If you avoid further contact with the triggering agent, your contact dermatitis will usually resolve on its own in two to four weeks following exposure. Common causes of contact dermatitis include:[1]
- Soap, cosmetics, nail polish, hair dyes, deodorant, or other personal care products
- Poison Ivy
- Bleach
- Nickel in jewelry and/or buckles
- Certain medical creams such as topical antibiotics
- Formaldehyde
- A recent tattoo and/or black henna
- Perfume
- Sunscreen
- Rubbing alcohol
-
2Wash the rash with warm water and mild soap. Before applying any topical treatments, be sure to first wash the area with warm (not hot) water and a gentle soap. This will ensure you remove any remaining traces of the possible trigger for your rash.[2]Advertisement
-
3
-
4Avoid using too much soap, makeup, or personal cosmetics, if these aggravate your contact dermatitis. Many hand soaps contain harsh ingredients and, as such, may exacerbate symptoms contact dermatitis (particularly if your contact dermatitis rash is present on your hands and/or lower forearms). If you find soap aggravating, minimize your use of soap while your rash recovers. Consider opting for a more mild cleanser, and use it sparingly until your rash improves.[5]
- Also avoid other cosmetics and personal hygiene products that trigger your contact dermatitis.
- If you are looking to replace cosmetics that you have noticed irritate your dermatitis, look for ones with a label that says "hypoallergenic" as these are less likely to trigger contact dermatitis. You may also want to consider switching to organic skin products.
- Even if you have been using the same products for years, sometimes formulas can change and a new additive might be causing new symptoms.
-
5Soothe your skin with cool, wet compresses to minimize irritation. Especially if your rash is crusting over and/or oozing fluid, wet dressings can be very effective. They may help to remove the crusts and diminish the itchiness and irritation.[6]
- Apply the compress for 15 to 30 minutes.
- If the contact dermatitis rash is widespread over your body (such as affecting both legs, both arms, or your trunk), one of the easiest solutions is to wear a wet piece of clothing.
- For instance, you may wear wet long johns with dry pants overtop, so that the moisture remains in contact with the affected areas of skin.
- The piece of clothing that you get wet will of course depend upon the area of your body that is affected.
- Change wet garments at least every eight hours.
- Use them as needed to soothe and ease symptoms.
-
6
-
7Do not use topical antihistamines. Topical antihistamine creams may actually worsen contact dermatitis and further aggravate the area of concern. As a result, it is not a treatment that doctors advise. Oral antihistamines, however, can help calm your symptoms, especially in allergic contact dermatitis.[8]
Opting For Medical Treatment
-
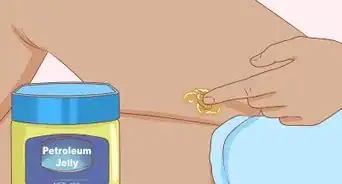
1Opt for a steroid cream. If basic self-care measures are insufficient to get your rash under control, your doctor may suggest an over-the-counter or prescription steroid cream. In the United States, Hydrocortisone cream is available over-the-counter in a strength of 1%; however, prescription steroid creams are available at higher strengths, and are thus more effective.[9]
- Note that steroid creams are most effective when you cover the area of the rash after applying the cream. This ensures that the cream remains on the location of interest, and is able to have an effective medicinal effect.
- Examples of coverings you can use over top of the steroid cream include a plastic wrap, petroleum jelly, or a dressing such as Telfa.
-
2Try medications that directly target your immune system. There are creams and ointments available that can directly target your immune system and help to repair your damaged (and irritated) skin. Examples include Tacrolimus/Protopic and Pimecrolimus/Elidel (both are calcineurin inhibitors).[10]
- These are not available over-the-counter, and must be prescribed by your physician.
- These are rarely given except for in very severe cases of contact dermatitis, as there is an FDA warning about a possible link between these immune-stimulating creams and ointments and certain types of cancer.
-
3Use oral corticosteroids for very severe cases. In the most severe cases of contact dermatitis — cases that do not resolve with a combination of self-care methods and steroid creams — your doctor may advise a short course of oral corticosteroids. It is not advisable to take oral corticosteroids for long periods of time due to the numerous side effects; however, used over the course of a few days, they may greatly help to get your rash under control.[11]
- An example of an oral corticosteroid is Prednisone.[12]
-
4Ask your doctor for antibiotics if your rash has become infected. As your rash/reaction heals following exposure to the triggering substance, it is key to keep an eye on it and to monitor for any signs of possible complications such as an infection. If your rash does become infected, your doctor will need to prescribe you a course of antibiotics to help combat the infection. It is important that you finish the full course of antibiotics, and do not miss any of the pills, even if your symptoms begin to resolve within a few days (as failure to do so could lead to the infection returning). Signs that your rash may be infected include:[13]
- You develop a fever
- Pus begins to ooze from your rash
- You develop fluid-filled blisters (as these may contain infectious material)
- Your skin becomes warm and red
Recognizing and Diagnosing Contact Dermatitis
-
1Recognize the signs and symptoms of contact dermatitis. Contact dermatitis is a skin reaction to something that your skin has been in contact with. This means the distribution of the rash/reaction will be where your skin was in direct contact with the triggering substance or object. For instance, it may be where your skin brushed up against poison ivy, or where a certain triggering metal from a piece of jewelry was in contact with your skin. Signs and symptoms to be on the lookout for include:[14]
- Reddening of the skin
- Bumps on the skin (most often red in color)
- Dry, cracked, or scaly skin
- Swelling over the affected area
- Painful, tender skin over the affected area
- Sometimes a burning sensation of the skin over the affected area
- Sometimes blisters that may ooze fluid and subsequently crust over (in more severe cases)
-
2Familiarize yourself with the different causes of contact dermatitis. There are two types of contact dermatitis, irritant and allergic, plus a number of different conditions that may resemble contact dermatitis. Irritant dermatitis is caused by something that physically, mechanically, or chemically, which disrupts the skin barrier. Allergic dermatitis is caused by something that triggers an auto-immune reaction. Allergic reactions do not show up immediately after exposure — it may be 12 to 48 hours before you react, or it may take repeated exposures (sometimes over a period of years) for a rash to appear. There are many things that can cause a reaction, so it may be difficult at first to figure out what is causing the rash.[15]
-
3Think back to recent exposures when attempting to diagnose the cause. If you look at the specific area of skin that is affected, you may be able to trace back the cause of your contact dermatitis. Think about objects or substances that have been in contact with the affected area of your body recently, that are unusual or "outside the norm" for you. It is possible that any of these things could be the offending agent.[16]
- Note that contact dermatitis often gets worse with time — that is, the more times you are exposed to the offending substance, the worse your rash/reaction will be.
- This is because it is an "adaptive immune response," meaning that your immune system stores the "memory" of the triggering agent and reacts more aggressively each time you are exposed to the triggering agent.
-
4See your doctor to confirm the diagnosis of contact dermatitis, and to receive treatment as needed. It is especially important to see your doctor if the rash becomes very painful and uncomfortable, interfering with your daily routine and/or with your ability to sleep. Also, if the rash affects your face or genitals it is key to see a physician for evaluation and treatment. Finally, if your rash shows no improvement after two to three weeks following exposure to the triggering agent, seek medical help by booking an appointment with your family doctor.[17]
References
- ↑ https://my.clevelandclinic.org/health/diseases/6173-contact-dermatitis
- ↑ https://medlineplus.gov/ency/article/000869.htm
- ↑ https://medlineplus.gov/ency/article/000869.htm
- ↑ https://www.aafp.org/afp/2010/0801/p249.html
- ↑ https://www.uptodate.com/contents/contact-dermatitis-including-latex-dermatitis-beyond-the-basics
- ↑ https://www.fairview.org/Patient-Education/Articles/English/c/o/n/t/a/Contact_Dermatitis_115897en
- ↑ https://www.uptodate.com/contents/contact-dermatitis-including-latex-dermatitis-beyond-the-basics
- ↑ https://www.uptodate.com/contents/contact-dermatitis-including-latex-dermatitis-beyond-the-basics
- ↑ https://medlineplus.gov/ency/article/000869.htm
- ↑ https://emedicine.medscape.com/article/1049216-medication#2
- ↑ https://www.aafp.org/afp/2010/0801/p249.html
- ↑ https://emedicine.medscape.com/article/911711-treatment#d12
- ↑ https://medlineplus.gov/ency/article/000869.htm
- ↑ https://www.fairview.org/Patient-Education/Articles/English/c/o/n/t/a/Contact_Dermatitis_115897en
- ↑ https://www.uptodate.com/contents/contact-dermatitis-including-latex-dermatitis-beyond-the-basics
- ↑ https://nationaleczema.org/eczema/types-of-eczema/contact-dermatitis/
- ↑ https://my.clevelandclinic.org/health/diseases/6173-contact-dermatitis
About This Article
To treat contact dermatitis, first wash the rash with warm water and mild soap to remove all traces of the rash trigger. Next, try using a moisturizing cream to soothe the itchiness. Calamine lotion has been found to work well. For further relief, try pressing a cool, wet compress over the rash for 15 to 30 minutes. However, if your contact dermatitis is widespread over your body, try wearing a wet piece of clothing instead. If the rash becomes very painful or starts interfering with your daily life, see your doctor for help. For more advice from our Medical reviewer and information on available medical treatments, read on!








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...