This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 33 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 9,021 times.
Bone density decreases with age and can lead to osteoporosis. It's important to have your bone density checked once you've reached a certain age or if you have other conditions that put you at risk for osteoporosis. Talk to your healthcare provider about bone density tests, learn how to interpret the results, and take steps to prevent bone loss to keep your body strong and healthy.
Steps
Discussing Test Options with Your Doctor
-
1Tell your doctor about your family history and any height loss or fractures. Be sure to tell your doctor of any family history of osteoporosis, as this increases your risk. Also let them know if you have recently broken a bone or have experienced height loss because these are signs of decreased bone density.[1]
- Other risk factors include low body weight and a small frame.
- Bone density decreases with age, and women are especially at risk of osteoporosis.
-
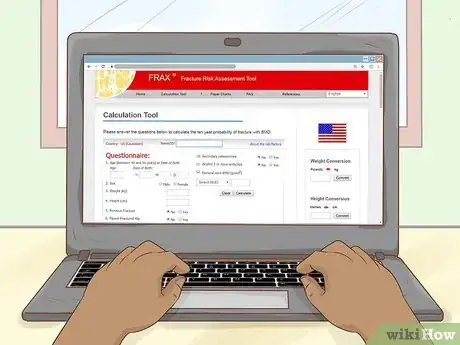
2Calculate your risk of bone fracture with the FRAX tool. This calculation does not replace the bone density test, but it can help you and your doctor make decisions about your bone health. FRAX calculates your risk of fracture based on factors like age, height, weight, race, ethnicity, nationality, and previous fractures. Ask your doctor about a FRAX calculation.[2]
- If you are between the ages of 40 and 90, you can also use the FRAX tool yourself by visiting https://www.sheffield.ac.uk/FRAX/index.aspx and selecting your country from the column “calculation tool.”
Advertisement -
3Request a DXA scan if you are a woman 65 years old or over. A dual-energy x-ray absorptiometry (DXA) machine is used to examine the density of your bones in your hips and spine—the bones people with osteoporosis are most likely to break. The test is non-invasive, painless, and only takes 10 to 15 minutes. In the US, many insurances won’t pay for DXA scans for men, because there is insufficient evidence on whether the tests benefit men.[3]
- A DXA test uses very little radiation—about the same amount you would get from having your hand x-rayed.[4]
- If you’ve had a DXA test before, try to get it at the same place so you clearly can see the changes in the test, rather than changes in the doctor’s method of reading the test.
-
4Ask for a peripheral exam as a precursor or if you’re over 300 pounds. Peripheral screenings can be used to measure bone density on your arms, wrists, fingers, or heels when DXA is not available or if you have certain conditions. The three types, pDXA (peripheral dual energy x-ray absorptiometry), QUS (quantitative ultrasound), and pQCT (peripheral quantitative computed tomography), can help determine if you need further testing.[5]
- Since most central DXA machines can’t test people over 300 pounds (140 kg), peripheral tests are often used instead.
- Peripheral tests are useful when you’re not sure if you need a full DXA test. For instance, if you are middle-aged with a small frame and are curious about your bone health or if your doctor doesn’t think you need a full scan depending on your age and risk factors.
- You can get a peripheral scan at certain drugstores, mobile health vans, and at health fairs.[6]
Completing the Procedure
-
1Refer to your insurance plan or doctor to schedule the test. Bone density tests require a referral from your healthcare provider, so they’ll likely recommend a certain hospital or testing center. However, it’s important to check in with your insurance plan to find a center in your network.[7]
- You can get a bone density test at private radiology centers and at hospitals that have radiology departments.
- If you have had any tests involving barium (like a swallow test with your gastroenterologist) or radioisotopes (like an MRI or thyroid scan) within the last 30 days, schedule your test to a later date as these elements may interfere with your results.
- Take your doctor’s referral note with you to your testing appointment. They’ll need your doctor’s information so they can send them the results.
-
2Eat normally and take any prescribed medications the day of the exam. Luckily, a bone density test requires very little preparation and you won’t have to change your usual routine. However, avoid taking any vitamins or supplements on the morning of your test.[8]
- Avoid taking calcium supplements for 24 hours before your test.[9]
-
3Wear comfortable clothing that doesn’t have metal components. You can remain fully clothed for the scan, but you have to remove any jewelry and clothing with metal fasteners like zippers, hooks, or buckles. You’ll also need to remove any metal objects from your pockets (like keys, coins, or money clips).[10]
- Loose, comfortable workout clothes are a good option.
- If most of your clothes have metal components, don’t worry, they’ll give you a gown to wear.
-
4Lie down on the scanning table and be still for 10-20 minutes. Be on time or early for your appointment so you can get checked in and registered. The technologist will then have you lay down on a scanning table for about 10-20 minutes while an arm of the DXA machine scans your spine and hips.[11]
- The technician may ask you to move your leg position so the scanning arm can reach a different area.
- If you’re getting a DXA-CT scan for 3D imaging, you’ll lie down on a table that moves into a cylindrical machine where it will scan your bones for about 10 minutes. If you’re claustrophobic, ask the technician or nurse to play some music for you or tell you jokes to distract you. You can also do a calming meditation beforehand.
-
5Wait 1-3 days for your doctor to share your results. A radiologist will analyze the results of your scan and send a report to your doctor. Expect to hear from your doctor anywhere from 1-3 days (depending on where you go to get the exam). Your doctor will then call you to discuss the results and, if necessary, ask you to come in for a follow-up appointment.[12]
- Some doctors email their patients instead or might provide a login and password to an online portal showing your results.
Reviewing Results and Treatment Plans
-
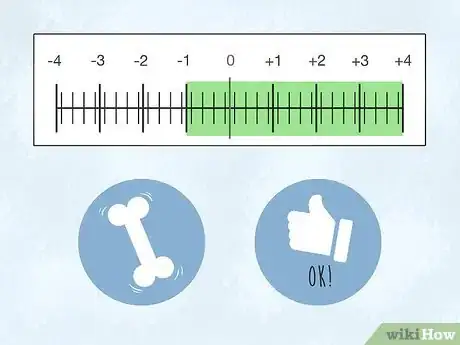
1Keep up the good work if your T-score is between -1 and +4. The T-score is determined by a formula that compares bone density to that of an average 30 year old. If instance, if your score is 0, your bones are the exact density that’s to be expected of a person that age.[13]
- If your T-score falls between -1 to +4, your bones are considered to be of normal density.
- A score of -1 doesn’t mean your bones are withering, it could mean you just have a small frame. However, your doctor might recommend that you get scanned again in a year or two just to make sure.
- If your score is +1 to +2, your bone density is 10% to 20% greater than that average—your bones are in great shape!
-
2Shift your diet and lifestyle and consider medication if your T-score is between -1 and -2.5. This score is typically means you have osteopenia. Don’t worry, osteopenia isn’t serious—it just means your bones are 10% to 25% less dense than an average 30 year old’s bones. Osteopenia doesn’t mean you’ll definitely get osteoporosis, it just means you have low bone density at the moment. Your doctor may consider putting you on medication if your T score is between -1 and -2.5 and they calculated a high probability that you’ll get a fracture using the FRAX tool.[14]
- If your bone density falls within this range, it’s time to make dietary and lifestyle changes to prevent bone loss and lower your risk of osteoporosis.
- If this is your first bone density test, your doctor won’t be able to tell if you’ve lost bone density or if you’ve always had (and probably will continue to have) low bone density due to your family or medical history. In this case, your doctor will request labs to try to determine whether or not you’re currently losing bone density.
-
3Take medication for osteoporosis if your T-score is -2.5 to -4. A score in this range means your bones are extremely porous and you are at high risk for fractures. Your doctor will typically prescribe medication like Atelvia, Boniva, or Actonel to help rebuild your bones.[15]
- Depending on your circumstances, your doctor may also suggest bi-annual intravenous infusions of zoledronic acid.
- Alter your diet and lifestyle to help rebuild your bones—your doctor can help you come up with a treatment plan.
Keeping Your Bones Healthy
-
1Quit smoking cigarettes to save your bones. Smoking affects the cells in your body that build bones and rejuvenate bones, which means smokers are more susceptible to osteoporosis.[16] Furthermore, smoking depletes your body’s store of vitamin C, which is necessary for calcium absorption and healthy bones.[17]
- Quit smoking cold turkey or wean yourself off of tobacco by decreasing the amount of cigarettes you smoke each day. You can also use nicotine gum, lozenges, patches, and sprays to ease withdrawal symptoms.[18]
- Chantix or Zyban are also two FDA-approved prescription drugs that can ease withdrawal symptoms while quitting.[19]
- Yoga and meditation can also help you curb cravings by being more present and aware of any triggers that lead you to smoke.[20]
-
2Avoid drinking alcohol in excess. Excessive drinking interferes with your body’s calcium and Vitamin D absorption. It may also mess up your body’s production of hormones and increase cortisol, which is linked to a higher risk of osteoporosis.[21] However, you can still indulge in moderation as mild drinkers have lower risk of fractures and bone loss.[22]
- Moderate drinking means 1 drink per day for women and no more than 2 drinks per day for men.[23]
- If you are older (50 and above) and struggle with alcoholism, you have an increased risk of fractures from falling.[24]
-
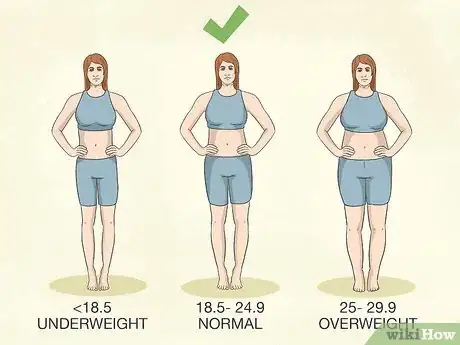
3Maintain a healthy weight. If your Body Mass Index (BMI) is below 18.5, you have a higher risk for bone loss than if you had a moderate BMI (ranging from 18.5 to 24.9).[25] Even mild obesity (BMI of 25 or more) can cause bone loss due to the deposition of fat into bone marrow.[26]
- Gain weight by eating a diet balanced in carbs, proteins, and fats. Calculate your daily caloric needs at https://bmi-calories.com/calorie-intake-calculator.html.
- Lose weight by eating a balanced diet (consisting mainly of whole foods), exercising, and practicing portion control.
-
4Stay active with at least 30 minutes of exercise 5+ days a week. Increasing your physical activity via aerobic exercise and resistance training can help build bone mass and decrease the risk of osteoporosis.[27] Incorporate strength training 3 out of 5 days a week, using moderate weights to target your glutes, back, shoulder, and arm muscles.[28]
- Focus on weight-bearing exercises like jumping jacks, jogging, hiking, stair climbing, and dancing. If you cannot do high-impact exercises, elliptical machines, stair step machines, and speed walking are great options for fragile joints.[29]
- If you already have osteoporosis, you can follow online exercises like this one: https://youtu.be/7fiqN8u5qYo?t=84. But always talk to your doctor before starting any new exercise program.
-
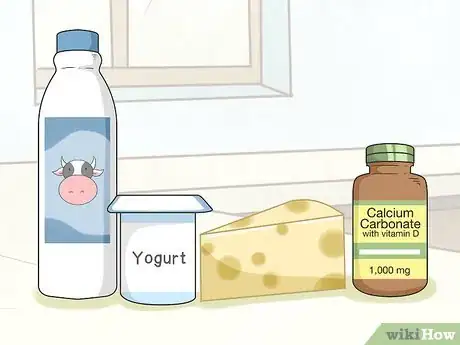
5Get enough calcium and vitamin D in your diet. Dairy products like milk, yogurt, and cheese are known for their calcium and Vitamin D content. However, green vegetables like collards, kale, broccoli rabe, and soybeans are additional sources. Orange juice, English muffins, soymilk, and cereals can also contribute to your daily intake as long as the package reads: “Fortified with calcium and vitamin D.”[30]
- Women 50 (and under) and men 70 (and under) need 1,000 mg of calcium and 600 IU of Vitamin D every day.
- Women over 51 and men over 71 should aim to get 1,200 mg of calcium and 800 IU of Vitamin D daily.
- You may need to take calcium supplements if you have a restrictive diet (i.e., if you’re vegan or have allergies to dairy or grains) and suspect you’re not getting enough calcium from food alone. Talk to your doctor before taking any supplements.
- Look for “fortified with calcium” on the labels of your favorite items.
- If a label only shows the percentage of daily value, interpret it as follows:
30% DV = 300 mg
20% DV = 200 mg
15% DV = 150 mg
-
6Eat lots of fruits and vegetables to lower your risk. People with a higher intake of fruits and vegetables have been shown to have greater bone density.[31] Leafy greens (like spinach and arugula) and cruciferous vegetables (like broccoli, brussels, collards, mustard greens, and cabbage), and citrus fruits (like oranges and grapefruits) can help you get enough calcium, magnesium, and vitamin C each day.
- Eat foods rich in Vitamin C along with foods rich in calcium increase absorption.[32] For instance, drink a glass of fortified orange juice before or with a meal full of greens and veggies.
-
7Get the right amount of protein. Foods with a lot of protein include red meat, poultry, seafood, eggs, and nuts. If you’re vegetarian or vegan, tofu, tempeh, seitan, beans, legumes, and plant-based protein powder are great options. To find your daily recommended intake of protein, multiply your weight by 0.36 and change pounds to grams.[33]
- For example, if you weigh 145 pounds (and live a sedentary lifestyle), you should aim to eat 52.2 grams of protein per day (and a few grams more if you regularly exercise).
- You can also use an online calculator: https://www.nal.usda.gov/fnic/dri-calculator/
-
8
Warnings
- Do not begin a new exercise program without talking to your doctor first, especially if you have osteoporosis.⧼thumbs_response⧽
- Don’t routinely repeat DXA scans more often than once every two years.⧼thumbs_response⧽
References
- ↑ https://www.nof.org/patients/diagnosis-information/bone-density-examtesting/
- ↑ https://www.sheffield.ac.uk/FRAX/index.aspx
- ↑ https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/osteoporosis-screening1#consider
- ↑ https://www.radiologyinfo.org/en/info.cfm?pg=safety-xray
- ↑ https://www.nof.org/patients/diagnosis-information/bone-density-examtesting/
- ↑ https://www.radiologyinfo.org/en/info.cfm?pg=dexa
- ↑ https://www.nof.org/patients/diagnosis-information/bone-density-examtesting/
- ↑ https://www.health.harvard.edu/medical-tests-and-procedures/bone-density-test-a-to-z
- ↑ https://my.clevelandclinic.org/health/diagnostics/10683-dexa-dxa-scan-bone-density-test
- ↑ https://www.nhs.uk/conditions/dexa-scan/what-happens/
- ↑ https://www.health.harvard.edu/medical-tests-and-procedures/bone-density-test-a-to-z
- ↑ https://www.health.harvard.edu/medical-tests-and-procedures/bone-density-test-a-to-z
- ↑ https://americanbonehealth.org/bone-density/understanding-the-bone-density-t-score-and-z-score/
- ↑ https://www.bonehealthandosteoporosis.org/patients/diagnosis-information/bone-density-examtesting/
- ↑ https://pubmed.ncbi.nlm.nih.gov/30919997/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28428669/
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/29644950
- ↑ https://www.bones.nih.gov/health-info/bone/osteoporosis/conditions-behaviors/bone-smoking
- ↑ https://www.fda.gov/consumers/consumer-updates/want-quit-smoking-fda-approved-products-can-help
- ↑ https://nccih.nih.gov/health/providers/digest/smoking-science
- ↑ https://pubmed.ncbi.nlm.nih.gov/21927919/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2692368/
- ↑ https://www.cdc.gov/alcohol/faqs.htm#excessivealcohol
- ↑ https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0180132
- ↑ https://www.bones.nih.gov/health-info/bone/bone-health/bone-health-life-health-information-basics-you-and-your-family
- ↑ https://www.frontiersin.org/articles/10.3389/fcell.2020.600181/full
- ↑ https://www.health.harvard.edu/womens-health/osteopenia-when-you-have-weak-bones-but-not-osteoporosis
- ↑ https://www.iofbonehealth.org/exercise-recommendations#Recommendations%20for%20young%20adults%20and%20pre-menopausal%20women
- ↑ https://www.nof.org/patients/fracturesfall-prevention/exercisesafe-movement/osteoporosis-exercise-for-strong-bones/
- ↑ https://www.nof.org/patients/treatment/calciumvitamin-d/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28045945/
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/1020374
- ↑ https://www.health.harvard.edu/blog/how-much-protein-do-you-need-every-day-201506188096
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3912260/
- ↑ https://pubmed.ncbi.nlm.nih.gov/29617220/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5728912/
- ↑ https://health.clevelandclinic.org/know-salt-hiding-food/








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...