This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 13 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 85% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 128,818 times.
The prostate gland is a part of the male reproductive system that can enlarge with age, putting uncomfortable pressure on the urethra. This can cause urinary difficulties, urinary tract infections (UTIs), and even bladder stones. By making lifestyle changes and using medication, most men can reduce their urinary troubles. A few men, though, may need to consider minimally invasive or traditional surgery options to feel their best.
Steps
Making Lifestyle Changes
-
1Reduce the amount of caffeine, soda, and alcohol you consume. Cut down on the amount of coffee, tea, soda, and alcoholic beverages you drink every week. Carbonation and caffeine can irritate the bladder, worsening urinary symptoms.[1]
- Try to drink no more than 200 milligrams of caffeine daily—about the amount in 2 cups of coffee. That’s about half the maximum amount for a healthy adult.[2]
- Drink no more than 4 alcoholic drinks in a given day or 14 drinks in a given week. It’s best to reduce your alcohol consumption as much as possible.[3]
-
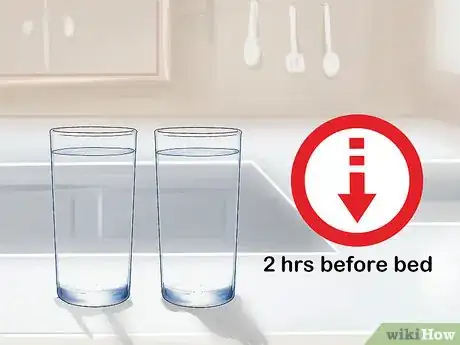
2Drink less liquid in the 2 hours before bed. Avoid drinking excess liquid in the evenings before you go to sleep. Going to bed with an empty bladder can help you avoid urinary discomfort and frequent urges overnight.[4]
- Increase your fluid intake earlier in the day to make sure you are drinking enough overall.
- Men should aim to drink 15.5 cups (3.7 liters) of fluid a day.[5]
- If you exercise strenuously or the weather is very hot, increase your fluid intake accordingly.
Advertisement -
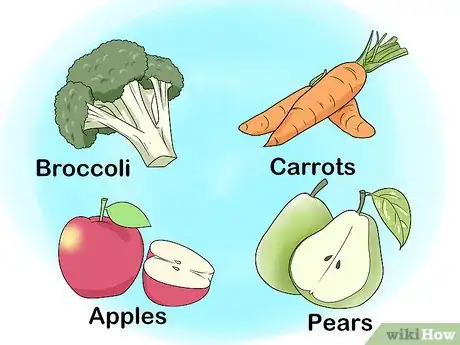
3Eat fiber-rich foods to encourage regularity. Eat more fiber-rich foods, such as fruit with the skin on, vegetables, lentils, nuts, and beans, to ward off constipation. Constipation can worsen enlarged prostate symptoms and put additional pressure on your bladder.[6]
- Fiber-rich fruits and vegetables include broccoli, apples, pears, carrots, Swiss chard, raspberries, and strawberries.[7]
- Men should get 30–38 grams (1.1–1.3 oz) of fiber per day depending on their age. While fiber supplements are safe, they can cause constipation. Aim to get your fiber from your diet rather than supplements whenever possible.[8]
-
4Try the double-voiding technique to empty your bladder fully. Wait about 30 seconds after you’ve finished urinating before trying to urinate again. Avoid straining or pushing. This can help you empty your bladder fully and reduce the frequency of UTIs.[9]
-
5Consult your doctor about side effects of your current medications. Talk to your doctor if you notice urinary troubles after starting another medication for an unrelated condition. Certain decongestants and antidepressants may aggravate urinary symptoms or cause prostate enlargement.[10]
- Your doctor can advise if there is a different medication you should try that would manage your condition without causing prostate problems.
- Avoid stopping any prescribed medication without consulting your doctor.
Using Medication to Reduce Symptoms
-
1Recognize the symptoms of an enlarged prostate. Look for a weak stream of urine, dribbling at the end of urination, or an increased need to urinate at night. You may also have difficulty starting urination or need to strain to empty your bladder. If you notice these symptoms, make an appointment with your doctor for an official diagnosis.[11]
-
2Try alpha-blockers if you have trouble urinating. Talk to your doctor about alpha-blockers, which can relax muscles around the bladder and prostate. These drugs help increase the flow of urine when you use the bathroom and keep you from needing to urinate too frequently.[12]
- While adverse side effects are infrequent, alpha-blockers can cause dizziness. The good news is, they typically help relieve symptoms within a few weeks.
- Take alpha-blockers, like tamsulosin, as directed by your doctor.
- Most alpha-blockers are safe to take with other medications. Consult your pharmacist for any potential drug interactions with your current medication regimen.
-
3Explore enzyme-inhibitors if you have a very enlarged prostate. Ask your doctor if enzyme-inhibitors, like finasteride and dutasteride, would be a good fit for your symptoms. These drugs shrink prostate tissue to reduce urinary problems and are often most effective on severely enlarged prostates.[13]
- Enzyme-inhibitors can take many months to improve your symptoms, as the prostate tissues shrink gradually over time.
- Like alpha-blockers, dizziness is the most common side effect.
- Talk to your pharmacist to make sure your enzyme-inhibitor will not interact negatively with your current medication regimen.
-
4Try Tadalafil if you have erectile dysfunction (ED). Talk to your doctor about Tadalafil, an erectile dysfunction drug, which has shown to be effective at also relieving urinary symptoms from an enlarged prostate. While you do not have to have ED to try Tadalafil, an enlarged prostate and ED are both common in aging men. If you suffer from both, this drug could resolve multiple symptoms.[14]
- The way that Tadalafil relieves urinary symptoms is not well understood, but adverse effects are infrequent. The most common are back pain and headaches.[15]
- How long Tadalafil takes to work on symptoms can vary from person to person. Discuss what to expect with your doctor.
- Tadalafil is not recommended with some other medications, including nitroglycerin. Consult your pharmacist for any potential drug interactions that may affect you.
Considering Surgical Treatments
-
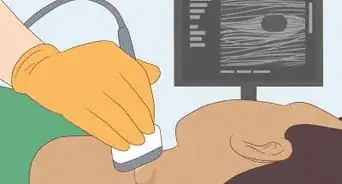
1Consider Transurethral Microwave Therapy (TUMT) for frequency and urgency. Discuss TUMT with your doctor if you have trouble with straining, urgency, or intermittent urine flow. This in-office procedure uses microwaves to destroy select portions of prostate tissue that are causing urinary blockages.[16]
- TUMT will not correct any bladder-emptying issues and is best for mild-to-moderate prostate blockages.
- Most discomfort from TUMT can be managed with topical anesthetic and oral pain medication in the doctor’s office.
-
2Discuss Transurethral Radio Frequency Needle Ablation (TUNA) to improve flow. Ask your doctor about TUNA, which destroys problematic tissue with high-frequency radio waves for a better flow of urine. The procedure involves needles being inserted directly into the prostate to target tissue compressing the urethra.
- This procedure is often done in a hospital setting but does not require a hospital stay. Local anesthesia is used to manage pain.
- Some side effects are possible after the procedure, including painful or frequent urination for a few weeks.
-
3Ask about a prostatic stent if surgery and medication aren’t for you. Talk to your doctor about a prostatic stent, which is a small coil inserted into the urethra to keep it open. Most doctors do not prefer stents, but if you have severe enlargement and don’t want to manage symptoms with drugs or other procedures, it can be a viable option.[17]
- Stents can shift position over time, causing further discomfort or urinary tract infections. They can also be difficult to remove if they are problematic.
-
4Discuss more invasive surgical options, if needed. Talk over surgical options with your doctor if your symptoms are not well-managed on medication or after minimally invasive procedures. While surgical procedures can sound intimidating, they often provide the most complete symptom relief.
- Your doctor can discuss the best surgical options for you given your urinary symptoms and medical history. Depending upon your age and fertility needs after the surgery, your doctor may present different options for treating your enlarged prostate.
- Common surgical options include prostatectomy, laser surgery, and transurethral incision or resection of the prostate.[18]
References
- ↑ https://www.nhs.uk/conditions/prostate-enlargement/treatment/
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/caffeine/art-20045678
- ↑ https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-your-drinking-pattern-risky/Whats-Low-Risk-Drinking.aspx
- ↑ https://www.nhs.uk/conditions/prostate-enlargement/treatment/
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256
- ↑ https://www.nhs.uk/conditions/prostate-enlargement/treatment/
- ↑ https://www.webmd.com/cholesterol-management/features/fiber-groceries
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983?pg=2
- ↑ https://www.nhs.uk/conditions/prostate-enlargement/treatment/
- ↑ https://www.nhs.uk/conditions/prostate-enlargement/treatment/
- ↑ https://www.mayoclinic.org/diseases-conditions/benign-prostatic-hyperplasia/symptoms-causes/syc-20370087
- ↑ https://newsnetwork.mayoclinic.org/discussion/enlarged-prostate-many-options-to-treat-this-common-problem/
- ↑ https://newsnetwork.mayoclinic.org/discussion/enlarged-prostate-many-options-to-treat-this-common-problem/
- ↑ https://newsnetwork.mayoclinic.org/discussion/enlarged-prostate-many-options-to-treat-this-common-problem/
- ↑ https://www.medpagetoday.com/urology/bph/10594
- ↑ https://www.mayoclinic.org/tests-procedures/tumt/home/ovc-20233737
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/17143103
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3989824/
- ↑ https://www.consumerreports.org/enlarged-prostate/reasons-to-skip-saw-palmetto-for-enlarged-prostate/












-Step-13.webp)



-Step-8-Version-3.webp)



















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...