This article was medically reviewed by Erik Kramer, DO, MPH and by wikiHow staff writer, Christopher M. Osborne, PhD. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 10,093 times.
Prostaglandins (PGs) are bioactive lipids that play numerous roles in important body functions, such as blood vessel constriction, muscle contraction, blood clotting, pain sensation, and inflammation.[1] Having too many PGs in your system, however, can cause excessive pain and inflammation. If your doctor determines by evaluation or blood testing that you have excessive PGs, work to reduce them by making dietary and lifestyle changes. Taking certain medications and supplements may also help reduce PGs.
Steps
Adjusting Your Diet
-
1Increase your fiber intake by eating more fruits and veggies. The fiber found in fruits and vegetables essentially works like a sponge, soaking up and removing things from your body as it works its way through your system. There’s growing evidence that fiber can soak up and remove excess PGs from your system as part of this process.[2]
- For example, fiber is known to remove excess estrogen. High estrogen levels increase the thickening of the uterine lining during the female menstrual cycle, which in turn increases PG production and, therefore, menstrual pain.
- Talk to your doctor before using fiber supplements to increase your intake.
-
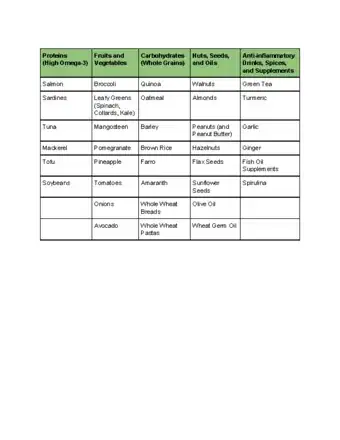
2Eat certain foods that may reduce PG levels. The evidence varies on the impacts of particular foods on the production of PGs. However, it may be worth trying some or all the following foods, all of which are good for your overall health:
- Foods rich in omega-3 fatty acids, including salmon, walnuts, and tofu.
- Vitamin E-rich foods like peanuts, almonds, broccoli, and avocados.
- Whole grains such as oatmeal, brown rice, and quinoa.
- Pineapples, pomegranates, and mangosteens.
- Onions, garlic, and tomatoes.
- Turmeric and ginger.
- Green tea.
Tip: Try switching to a low-fat, high-fiber vegan diet since it has been shown to significantly reduce pain in women reducing PGs.
Advertisement -
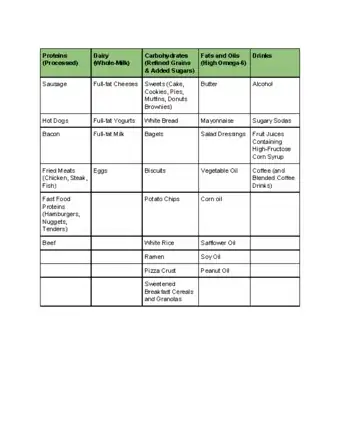
3Reduce your intake of unhealthy fats to cut PG production. For females in particular, reducing fat intake reduces estrogen production, which in turn reduces PG production. In any case, reducing your fat intake—and especially your intake of saturated fat and other unhealthy fats—will benefit your overall health.[3]
- A female who cuts her fat intake by 50% may reduce her estrogen production by 20%.
- Foods high in saturated fat include red meats, processed meats, fried foods, fast foods, packaged processed foods, and full-fat dairy products.
- While cutting back on your overall fat intake, make sure to still include some amount of healthy fats, such as those in olive oil, avocados, and nuts, in your diet.
- Talk to your doctor before drastically changing your diet, such as by dramatically cutting your fat intake.
-
4Cut back on added sugars, omega-6 fatty acids, and alcohol. Consuming any of these in excess may increase the production of PGs. And, in any case, cutting back is a good choice for your overall health.[4]
- It’s possible that added sugars in things like candies, pastries, and sugary beverages may increase inflammation and PG production.
- Omega-6 fatty acids, which are particularly found in oils like vegetable, safflower, corn, soybean, and peanut, may contribute to increased PG production. Don’t confuse these with omega-3s (found in foods like salmon and walnuts), which may help decrease PG production.
- Drinking excessive amounts of alcohol—averaging more than 1 alcoholic drink per day for females and 2 per day for males—might increase your body’s production of PGs.
Taking Medications
-
1Take NSAIDs to cut PGs in response to injury or inflammation. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Motrin) and naproxen (Aleve) block enzymes that produce PGs in response to injury or inflammation. Cutting PGs helps to reduce your experience of pain and further inflammation.[5]
- For occasional pain relief, use NSAIDs exactly as directed on the packaging. Consult your doctor or pharmacist before taking an NSAID if you take prescription medications or have pre-existing health conditions.
- Do not use NSAIDs as a long-term treatment without your doctor’s approval and monitoring.
- You can start taking NSAIDs for pain at the start of your menstruation and take them during that time. Wait until your following cycle to start taking them again to reduce PGs.
-
2Discuss using aspirin to reduce PGs related to blood clotting. Like NSAIDs, aspirin blocks the production of certain PGs, which aids in pain relief. However, aspirin is particularly effective at blocking PGs that are associated with blood clotting, which is why it is sometimes prescribed as a daily treatment for people with heart conditions or clotting disorders.[6]
- Do not use aspirin as a daily therapy unless prescribed by your doctor. It can increase your risk of internal bleeding, among other side effects.
- Talk to your doctor before using aspirin as an occasional pain reliever, especially if you’re at risk for internal bleeding, have a clotting disorder, or are on any other anticoagulant medications.
- Do not give aspirin to children age 18 and younger.
-
3Consider oral contraceptives to cut PGs tied to menstrual pain. The endometrial cells that thicken a female’s uterine lining during the menstrual cycle produce a large amount of PGs in the process. Oral contraceptives limit the thickening of the uterine lining, which in turn reduces the production of PGs.[7]
- Reducing the number of PGs produced during your period may substantially decrease the amount of pain and discomfort you experience.
- Discuss the pros and cons of using an oral contraceptive with your doctor. They’re very effective (but not foolproof) at preventing pregnancy, but may also slightly increase your risk of blood clots, strokes, heart attacks, and certain cancers.
-
4Watch for new developments in PG-reducing medications. As biomedical researchers learn more about the different types and functions of PGs, the possibility for new PG-reducing medications continues to grow. If any new treatment options reach the trial stage or hit the market, talk to your doctor about the potential pros and cons of trying such medications.[8]
- Keep in mind that there are always risks involved in the development of new medications. Vioxx, for example, was developed as a “selective” NSAID that targeted particular PGs. It was withdrawn from the market, however, because it increased the risk of heart attack and stroke beyond an acceptable level.
Trying Lifestyle Changes and Supplements
-
1Relieve excess stress to help reduce inflammation. Excessive stress can increase your body’s inflammatory response, and inflammation triggers the production of PGs that can cause pain and additional inflammation. So, if you effectively manage stress, you may be able to keep your PGs in check more effectively.[9]
- Try different healthy stress-relief activities until you find the ones that work best for you. These might include yoga, meditation or prayer, deep breathing exercises, outdoor activities, light exercise, a warm bath, calming music, or a good book.
- Talk to your doctor about seeing a mental health professional if you’re struggling to manage the stress in your life.
-
2Exercise to release endorphins and reduce pain. The endorphins released during exercise can improve your mood and reduce the amount of pain you experience. Following a regular exercise routine may also manage inflammation and the production of PGs.[10]
- Talk to your doctor before beginning a new exercise program, especially if you live a sedentary lifestyle or have existing medical conditions.
- With your doctor’s approval, aim for the following weekly goals as a healthy adult: 150+ minutes of moderate-intensity aerobic exercise (like biking or swimming); 2-3 strength-training sessions; and 2-3 flexibility training sessions.
-
3Talk to your doctor about supplements that may reduce PGs. The medical evidence is generally limited or inconclusive when it comes to the effectiveness of particular supplements in reducing PGs. Consult your doctor before trying any new supplements, as they can interact with medications and cause side effects. With your doctor’s approval, consider possible PG-reducing supplements like:[11]
- Fish oil.
- Manganese glycinate.
- Vitamin E.
- Iron.
- Multivitamins.
Lists of Foods That May Raise or Lower PGs
References
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4028977/
- ↑ https://www.pcrm.org/good-nutrition/nutrition-information/using-foods-against-menstrual-pain
- ↑ https://www.pcrm.org/good-nutrition/nutrition-information/using-foods-against-menstrual-pain
- ↑ https://www.arthritis.org/living-with-arthritis/arthritis-diet/foods-to-avoid-limit/food-ingredients-and-inflammation.php
- ↑ https://www.yourhormones.info/hormones/prostaglandins/
- ↑ https://www.yourhormones.info/hormones/prostaglandins/
- ↑ https://www.pcrm.org/good-nutrition/nutrition-information/using-foods-against-menstrual-pain
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4028977/
- ↑ https://www.sciencedirect.com/science/article/abs/pii/S0889159112004758













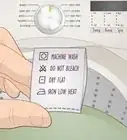
-Step-3-Version-3.webp)


















-Step-3-Version-3.webp)































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...