This article was co-authored by Alan O. Khadavi, MD, FACAAI. Dr. Alan O. Khadavi is a Board Certified Allergist and a Pediatric Allergy Specialist based in Los Angeles, California. He holds a BS in biochemistry from the State University of New York (SUNY) at Stony Brook and an MD from the State University of New York Health Science Center at Brooklyn. Dr. Khadavi completed his pediatric residency at Schneider Children’s Hospital in New York, and then went on to complete his allergy and immunology fellowship and pediatric residency at Long Island College Hospital. He is board certified in adult and pediatric allergy/immunology. Dr. Khadavi is a Diplomate of the American Board of Allergy and Immunology, a Fellow of the American College of Allergy, Asthma & Immunology (ACAAI), and a member of the American Academy of Allergy, Asthma & Immunology (AAAAI). Dr. Khadavi's honors include Castle Connolly’s list of Top Doctors 2013-2020, and Patient Choice Awards "Most Compassionate Doctor" in 2013 & 2014.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 94,216 times.
Many things can cause a swollen nose: a rhinoplasty, a pregnancy, an allergic reaction, a facial injury, or a broken nose. Fortunately, although a swollen nose can be a little painful and slightly embarrassing, it’s not a serious condition. Reducing nasal swelling is a relatively quick and easy process. Try applying ice to the swollen areas to decrease the swelling, and avoid irritants that inflame your nose. If the swelling remains, make an appointment with your doctor so they can assess your nose.
Steps
Relieving Pain Quickly
-
1Hold an ice pack to your nose for 10-15 minutes at a time. Fill a wet washcloth with 5-6 ice cubes. Then, apply the ice pack directly against the swollen part of your nose, and hold it in place with moderate pressure. Pressing too hard may be painful or further damage your nose. The cold from the ice will reduce the swelling. Once 10-15 minutes have passed, remove the ice pack.[1]
- If you prefer not to use a washcloth, you can purchase a plastic ice pack from a pharmacy. Place it in the freezer for 3-4 hours before using.
- Do not hold ice cubes directly against your nose, as they may stick to the skin or cause frostbite.
-
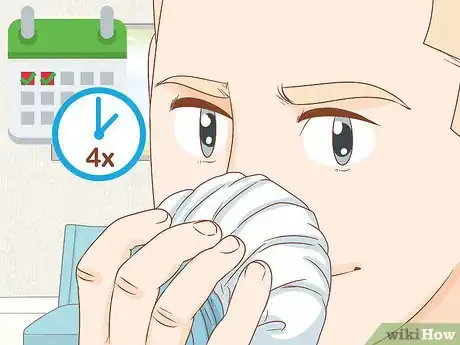
2Apply the ice pack 4 times a day for 1-2 days. If you’re awake for 16 hours of the day, hold the ice pack against your nose once every 4 hours.[2] Apply the ice pack at, for example, 9am, 1pm, 5pm, and 9pm. If your nose is still swollen after 24 hours, use the ice pack for the next 24 hours as well.
- Using the ice pack more than this will not be effective at decreasing swelling.
- Holding the ice pack against your nose will also help reduce any pain associated with the injury or rhinoplasty.
Advertisement -
3Take an over-the-counter pain reliever every 4-6 hours. NSAID pain relievers like Ibuprofen and Advil will reduce swelling in addition to decreasing the pain you may experience with a swollen nose.[3] Taking too much of an OTC pain medication can damage your body (especially your stomach), so carefully follow the directions printed on the medication’s packaging.
- Avoid taking more pain pills than directed on the bottle. For most OTC pain medicines, avoid taking more than 3,000 mg per day.[4] This is usually about 4 doses of the medication.
-
4Keep your head elevated while you sleep. Propping 1 or 2 extra pillows under your head will allow blood and other fluids to drain out of your swollen nose. When you awake after a night’s rest or a nap, your nose will be less painful and the swelling will also have subsided.[5]
- If you do not elevate your head when you rest, you may awake with a sore, throbbing, swollen nose.
Avoiding Irritants and Draining Sinuses
-
1Take an OTC nasal spray to counteract allergies.[6] During spring and fall, many people suffer from seasonal allergies. These allergies—and the frequent sneezing and nose-blowing that they bring about—can cause your nose to swell. Take the nasal spray as directed and spray the medication directly up your nose. Most should be taken once a day, with 1 or 2 sprays per nostril.[7]
-
2Avoid any allergens that cause your nose to swell. If your allergies are caused by a non-seasonal allergen, avoid the allergen. Some allergies to cosmetic products like facial creams, lotions, or soaps can cause nasal swelling. Stop using these products if this is the case.[10] Or, if you’re allergic to pets, avoid spending time in the houses of friends with pets.
-
3Stay away from pollutants that irritate and inflame your nose. Air pollution and smoke from cigarettes (and other tobacco products) can cause the mucous membranes inside of your nose to swell. Avoid environments that are filled with smoke, and stay indoors as much as possible on days with high pollution.[11]
- If you cannot stay indoors on pollution-heavy days, wear a surgical mask or bandana over your mouth and nose.
-
4Rinse your nose out with salt water to remove irritants. If you’re struggling to breathe through your nose, the inner membranes are likely swollen. Purchase a nose-rinsing pot from a local pharmacy, and follow the directions to rinse irritants out of your nose. Washing out the nasal passages with saline water will remove whatever irritants may be causing the swelling.[12]
- The medical term for swelling inside of your nose is rhinitis.[13] While this swelling is often limited to the mucous membranes in your nostrils, severe rhinitis can cause the entire nose to swell.
-
5Reduce the amount of salt and processed foods that you eat. Sprinkle less table salt on your daily meals and focus on eating healthy, whole foods that are low In sodium. Salt and unhealthy processed foods can make your body retain water and swell up. Reducing salt is especially useful if your nose swells during pregnancy, as several of the previous steps may not reduce your swelling.[14]
- Processed foods include things like tinned vegetables, American cheese, breakfast cereals, microwave-ready meals, and processed meats.
-
6Drink less caffeine throughout the day. The caffeine found in drinks like coffee, soda, and tea causes your body to retain water. If you’re pregnant or have recently had a rhinoplasty, some of this swelling may occur in your nose. Drinking sweet caffeinated drinks (especially soda) may worsen the swelling, since sugars also cause your body to retain water.[15]
- So, if you typically drink 3–4 cups of coffee or soda in the morning and afternoon, cut back to 1–2 cups.
Visiting a Doctor for a Broken Nose
-
1Schedule an appointment if you suspect that your nose is broken. If you received a blow to your nose and the nasal swelling (and any accompanying pain) haven’t gone away after 3-5 days, you should see a doctor. Also, make an appointment if you can feel the broken bones in your nose or if your nose looks crooked following the blow.[16]
- If swelling and pain from a rhinoplasty haven’t gone down after 5-7 days, call your plastic surgeon and ask what they recommend.
-
2Describe your symptoms to your doctor. Tell your doctor how and when you sustained an injury to your nose. Also, mention any symptoms you’ve been experiencing since. These may include headaches, nosebleeds, swelling, and general nose pain. Finally, tell your doctor if you have had trouble breathing since the incident, or if you’ve been unable to breathe through your nose altogether.[17]
- Your doctor will also want to know if you’re currently taking any prescription or over-the-counter medications.
-
3Get an X-ray to assess your broken nose. If your doctor can’t easily determine if your nose is broken, they may need to use 1 or more imaging scans to assess your nose. The doctor will likely order either an X-ray or a computed tomography (CT) scan for broken bones in your nose. These scans will allow the doctor a better view of the bones inside your nose.[18]
- Your doctor will also order an X-ray or a CT scan if they suspect that your face or skill may have sustained additional injuries from the injury that damaged your nose in the first place.
-
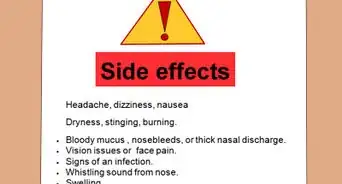
4See an ENT specialist if your nose is broken. If your general practitioner determines that your nose is broken, they’ll most likely refer you to an ears, nose, and throat (ENT) specialist.[19] The ENT doctor will be able to re-align the broken bones in your nose, situate the fragments so they’ll properly set, and pack your nose to prevent further damage. They may also request that you take antibiotics while the nasal fracture heals.[20]
- When deciding between ENT specialists, contact your insurance company and make sure that the specialist is in-network.
-
5Return to the ENT specialist after 2-3 days. If the ENT specialist packs and sets your broken nose, they’ll most likely want you to schedule a second appointment in this timeframe. During this follow-up appointment, the ENT doctor will inspect your nose, see if it’s healings and remove the packing gauze from your nose.[21]
- If the nasal break isn’t healing well, the ENT specialist may decide to apply a nasal splint to your nose.
References
- ↑ https://www.mayoclinic.org/diseases-conditions/broken-nose/diagnosis-treatment/drc-20370444
- ↑ https://www.mayoclinic.org/diseases-conditions/broken-nose/diagnosis-treatment/drc-20370444
- ↑ https://www.mayoclinic.org/diseases-conditions/broken-nose/diagnosis-treatment/drc-20370444
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK361006/
- ↑ https://www.mayoclinic.org/diseases-conditions/broken-nose/diagnosis-treatment/drc-20370444
- ↑ Alan O. Khadavi, MD, FACAAI. Board Certified Allergist. Expert Interview. 29 July 2020.
- ↑ https://www.medicalnewstoday.com/articles/319511.php
- ↑ Alan O. Khadavi, MD, FACAAI. Board Certified Allergist. Expert Interview. 29 July 2020.
- ↑ Alan O. Khadavi, MD, FACAAI. Board Certified Allergist. Expert Interview. 29 July 2020.
- ↑ https://www.medicalnewstoday.com/articles/319511.php
- ↑ https://www.buoyhealth.com/symptoms-a-z/swollen-nose/
- ↑ https://www.nhs.uk/conditions/non-allergic-rhinitis/treatment/
- ↑ https://www.nhs.uk/conditions/non-allergic-rhinitis/causes/
- ↑ https://www.unitypoint.org/livewell/article.aspx?id=e668bf44-c376-459e-b263-41f48810373
- ↑ https://www.unitypoint.org/livewell/article.aspx?id=e668bf44-c376-459e-b263-41f48810373a
- ↑ https://www.mayoclinic.org/diseases-conditions/broken-nose/diagnosis-treatment/drc-20370444
- ↑ https://www.mayoclinic.org/diseases-conditions/broken-nose/diagnosis-treatment/drc-20370444
- ↑ https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=nosei
- ↑ https://www.mayoclinic.org/diseases-conditions/broken-nose/diagnosis-treatment/drc-20370444
- ↑ https://www.peacehealth.org/medical-topics/id/nosei
- ↑ https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=nosei
- ↑ https://www.peacehealth.org/medical-topics/id/nosei
- ↑ https://www.medicalnewstoday.com/articles/319511.php




































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...