This article was medically reviewed by Erik Kramer, DO, MPH and by wikiHow staff writer, Jennifer Mueller, JD. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 94,954 times.
The human knee is composed of seven ligaments that go through and around the joint and it's compositional pieces. These ligaments are necessary to maintain stability in the body’s joints. Two of these ligaments are more vulnerable to injuries compared to others. These are the anterior cruciate ligament (ACL) and medial collateral ligament (MCL). The medial collateral ligament is located on the internal side of the knee joint. It adjoins the thigh bone and the shin bone. This type of knee ligament injury is very common among athletes. Recovery involves both medical intervention and at home recovery strategies.
Steps
Using Self-help Strategies
-
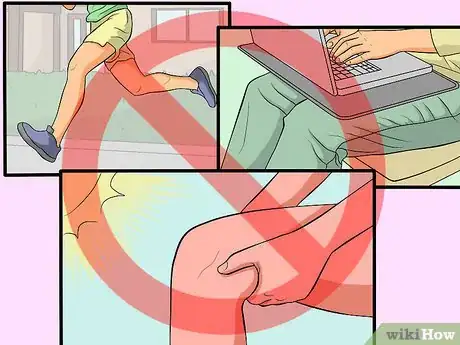
1Protect your knee from further damage. Limit the amount of moving around you do right after the injury occurs. Injured ligaments should be well rested to promote faster healing and to avoid further injury. Make sure to avoid placing any excessive pressure on your MCL, as this could cause further complications.
- Another way to avoid damaging your knee further is to avoid exposing your knee to hot temperatures for at least 48 hours after the injury occurs. Hot temperatures could cause your knee to swell up and become even more tender.
-
2Immobilize your knee. Your doctor may recommend that you wear a knee brace for a period of time (the length of time depends on how badly the knee was injured). A brace can help to keep your knee stable, which in turn can keep further damage from occurring.Advertisement
-
3Compress your knee.[1] Use an ice compress to do this. Cold temperatures can help to numb the area so you feel less pain, while also restricting the flow of blood to the area, which can help to bring the swelling down.
- Do not place an ice pack or ice directly against your skin;[2] make sure to wrap it in a hand towel first to avoid damaging your skin. Hold the ice pack against your knee for 15 to 20 minutes, then let your knee rest. You can repeat this process throughout the day.
-
4Elevate your knee.[3] You should elevate your knee above the level of your heart; doing this can help to keep the amount of swelling that occurs to a minimum. Continue to elevate your knee as much as possible for at least 48 to 72 hours after the injury occurs.
- You can use a pillow to prop up your leg.
Using Medical Intervention
-
1Take medications to control the pain caused by the sprain. In addition to managing the pain, you should also try to combat any swelling that occurs by taking either painkillers or NSAIDs[4] :
- Painkillers: These medications limit the pain impulses that are transmitted to your brain, so you don’t feel the pain as acutely. You can purchase simple painkillers, like Paracetamol, over-the-counter. If they don’t work to eliminate your pain, you can also get a prescription for stronger painkillers like codeine and tramadol from your doctor.
- Oral Non-steroidal Anti-inflammatory drugs (NSAIDs): These medications limit both pain and inflammation by acting on certain chemicals in your body. Common NSAIDs include Ibuprofen, Naproxen and Aspirin.
-
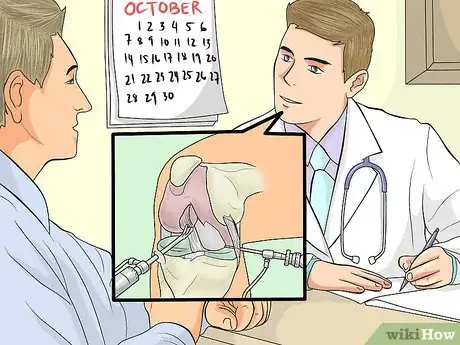
2Talk to your doctor about surgical management. Some people do not respond well to taking medications; if you are one of these people, you may want to consider correcting the damage through surgery.
- MCL sprains are commonly corrected with arthroscopic surgery; this surgery involves using a tiny camera to get a visual picture of the damaged area to help surgeons repair the sprain.
-
3Get a brace for your knee. A lightweight hinged knee brace can help to gradually increase your range of motion. The brace keeps your knee stabilized to prevent further injury.[5]
- As you recover, you may be given a different knee brace that can help you to begin using your knee again without putting too much pressure on the knee.
Strengthening Your MCL with Exercises
-
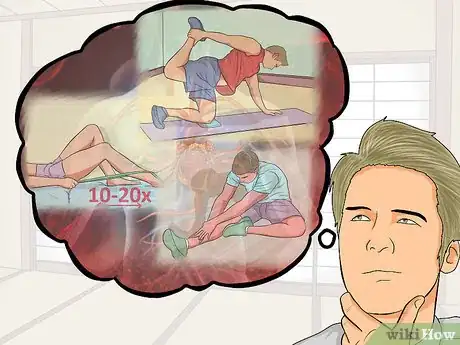
1Go see a physical therapist. There are certain exercises that are recommended for people who have suffered an MCL sprain. However, it is important to talk to a physical therapist before you try any of these exercises; if you begin these exercises too soon after your injury, you could cause further damage.
-
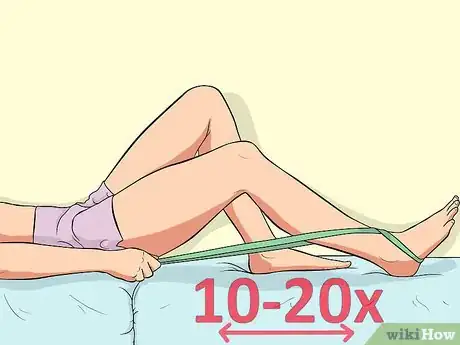
2Try a heel slide exercise. Assume a lying position with the injured knee in a bent position. Keep your foot flat on the floor and slowly slide the heel in the direction of your buttocks as far as you possibly can without it hurting.
- Repeat this exercise 10 to 20 times.
-
3Practice a quad stretch. Grasp the right foot with the right hand and gradually pull the foot up then behind your back, towards the buttocks. Reach as far as possible until a stretch is felt.
- Maintain this position for 10 seconds then return your leg to the starting position. Switch to your other leg and repeat the exercise.
-
4Do a hamstring stretch. In a standing pose, position one leg in front of the other leg. Bend the back knee while keeping the front knee straight. Place the weight on the bent knee and then lean forward. Stop once a stretch is felt at the back of the thigh
- . Hold this position for 5 to 10 seconds then return to the starting position. Switch legs and repeat the exercise.
-
5Understand why exercising your knee is important. Exercises and muscle movements promote good blood circulation and oxygen distribution to the affected area, thus speeding up the repair of the damaged tissue.
Understanding MCL Strains
-
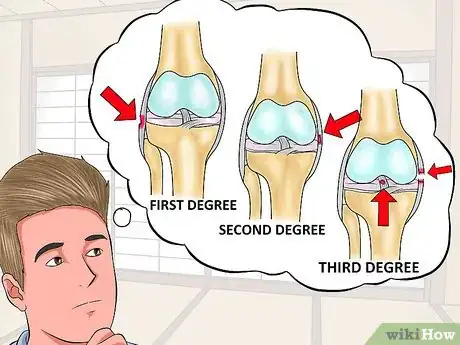
1Be aware that there are different kinds of sprains that can occur in the MCL. Sprain can be classified depending on the severity of damage to the ligament:
- First Degree Sprain: Only a small number of ligament fibres are damaged.
- Second Degree Sprain: Affects a greater portion of ligament fibres however the ligaments stay integral.
- Third Degree Sprain: Causes total shatter of the ligament that can affect other structures in the knee like the meniscus (cartilage) and Anterior Cruciate Ligament.
-
2Recognize the causes and risk factors of an MCL sprain. People who play contact sports where you collide with other players often suffer from this injury. However, this type of sprain can also be caused by any trauma that causes a disturbance to the ligaments.
- Athletes who participate in contact sports, or sports where they must run and change direction quickly are at a greater risk of injuring their MCLS.
-
3Look for symptoms of an MCL sprain. The signs and symptoms of an MCL sprain may vary depending on the degree of injury:
- First degree sprain: Localized sharp pain is felt on the site of injury due to the stress or irritation placed on the ligament. Sensation of pain may worsen upon movement of joints or after any contact made on the injured part.
- Second degree sprain: You may feel pain if the injured area is touched, or any pressure is applied to it. Inflammation may be visible within 24 hours after injury. The pain is sharp and throbbing or pulsating.
- Third degree sprain: Rupture of the ligament is present accompanied by unsteadiness of the knee joint. Any movement or activity involving the knee joint may be impaired as well. Swelling can be apparent due to the leakage of fluids from the damaged joint. The pain is sharp and excruciating.
References
- ↑ https://www.physio-pedia.com/Medial_Collateral_Ligament_Injury_of_the_Knee
- ↑ https://activewrap.com/blogs/news/common-mistakes-when-using-an-ice-pack
- ↑ https://www.ucsfhealth.org/conditions/mcl-tear/treatment
- ↑ Phipps, Cassmeyer, Sands, Lehman (1995) Medical Surgical Nursing 5th Edition
- ↑ Phipps, Cassmeyer, Sands, Lehman (1995) Medical Surgical Nursing 5th Edition







































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...