This article was medically reviewed by Mark Ziats, MD, PhD. Dr. Mark Ziats is an Internal Medicine Physician, Scientist, Entrepreneur, and the Medical Director of xBiotech. With over five years of experience, he specializes in biotechnology, genomics, and medical devices. He earned a Doctor of Medicine degree from Baylor College of Medicine, a Ph.D. in Genetics from the University of Cambridge, and a BS in Biochemistry and Chemistry from Clemson University. He also completed the INNoVATE Program in Biotechnology Entrepreneurship at The Johns Hopkins University - Carey Business School. Dr. Ziats is board certified by the American Board of Internal Medicine.
There are 10 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 77,900 times.
Experts agree that malaria is caused by a parasite that's transmitted through bites from infected mosquitoes. Malaria is most common in tropical and subtropical environments, so you're unlikely to catch it if you live in a temperate climate.[1] Research shows the most common symptoms of malaria are fever, chills, and flu-like symptoms, but you may develop complications if you don't get treatment.[2] If you suspect you have malaria, see a doctor immediately so you can start treatment.
Steps
Recognizing the Symptoms of Malaria
-
1Watch for a high fever. One of the primary symptoms that is so common with a malarial infection is a high fever, at least 102°F (38.9°C).[3] It's also one of the first symptoms to appear as early as seven days (although usually between 10 – 15 days) after getting bitten by an infected mosquito. Often the fever comes and goes randomly. This is thought to be related to the malaria parasites transiently spreading into blood from the liver.
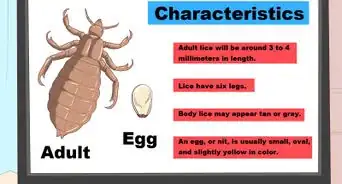
- There are at least five types of Plasmodium parasites that infect people, although P. falciparum (mainly in Africa) and P. vivax (mainly in Latin America and Asia) are the most common and deadly.
- The fever and other initial symptoms may be mild and mimic less serious viral infections, such as the common cold and influenza.
- Usually symptoms don't appear for about two weeks after being bitten.
-
2Take notice of severe shaking chills. The other primary symptom of malaria is severe shaking chills with intermittent periods of sweating.[4] Again, shaking chills are typical of many other types of infections, but they are usually more pronounced and severe with malaria. They can cause teeth to chatter and even prevent sleep. When they're severe, the shaking can be mistaken for seizures. The chills from malaria are usually not remedied by blanket cover or by wearing warmer clothes.
- Although the primary symptoms of malaria typically begin within a few weeks of being bitten by an infected mosquito, some types of malarial parasites can lie dormant in the body for up to a year or more.[5]
- Malarial symptoms are caused by the bites from female Anopheles mosquitoes, which inject the parasite into the host's bloodstream. The parasites then migrate to the liver where they lay dormant for a week or two before causing symptoms.
Advertisement -
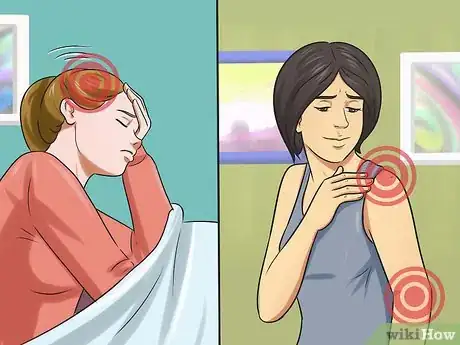
3Look out for headaches and muscle pains. Secondary and less specific symptoms of malaria are moderate-to-severe headaches, often combined with mild muscle aches.[6] These secondary symptoms often occur a short while after the above-mentioned primary symptoms as the parasite needs a little more time to proliferate in the liver and spread around the body in the bloodstream. Headaches and muscle aches are also very common with most other infections, as well as from the bites of other insects and spiders.
- The bites from female Anopheles mosquitoes are not very noticeable (a small, red, itchy bump), unlike the bites of some other insects and spiders that can cause similar symptoms.
- The initial headaches of malaria are typically dull in nature (like a tension headache), but as the parasites start to infect and destroy red blood cells, they can become pounding in nature (more like a migraine).
- The achy pain is usually most noticeable in the leg and back muscles because they are larger, more active and get more of the infected blood.
-
4Be suspicious of vomiting with diarrhea. Other non-specific secondary symptoms of malaria are vomiting and diarrhea, multiple times per day.[7] They often occur in combination with each other, which mimics the initial symptoms of food poisoning and other bacterial infections. The main difference is that the vomiting/diarrhea caused by food poisoning fades away within a few days, whereas it can remain for a few weeks with malaria (depending on treatment).
- Unlike the explosive and bloody diarrhea of some bacterial infections, particularly Shigella, there's usually no blood or severe cramping with malaria.
- Once the primary and secondary symptoms become noticeable, the malaria-causing parasites can be seen under a microscope from a drop of infected blood — especially if the specimen is stained with Giemsa stain.[8]
-
5Recognize the advanced symptoms. If the advancing primary and secondary symptoms don't prompt the infected person to seek medical attention and get treatment (which may not be possible in the developing world), then symptoms begin to appear that signify serious injury / damage to the body.[9] When these advanced symptoms of malaria appear, the risk of health complications and death significantly increase.
- Confusion, multiple convulsions, coma and neurological impairment indicate brain swelling and injury.
- Severe anemia, abnormal bleeding, deep labored breathing and respiratory distress indicate advanced blood infection and lung involvement.
- Jaundice (yellowish skin and eyes) is evidence of liver damage and dysfunction.
- Kidney failure
- Liver failure
- Shock (very low blood pressure)
- Enlarged spleen
Understanding the Risk Factors
-
1Be very cautious of underdeveloped tropical areas. The biggest risk factor for coming down with malaria is either living in or traveling to tropical countries where the infection is common.[10]
- The most risky areas are African countries south of the Sahara Desert, most of the Asian subcontinent, Haiti, Solomon Islands and Papua New Guinea.[11]
- The Centers for Disease Control and Prevention (CDC) estimate that 90% of all malaria deaths occur in Africa — mostly in kids younger than five years.
- Approximately 1,500 cases of malaria are diagnosed in the U.S. each year, mostly in returned travelers.[12]
-
2Be particularly careful if your immune system is weak. People with immature or weakened immune systems are especially susceptible of getting infected by Plasmodium parasites and developing malaria. This group includes infants, children younger than five years, pregnant women, the elderly and patients with HIV/AIDS.[13] As such, don't travel to high-risk countries if you are in this group and/or don't bring young children with you.
- Strong immune systems can fight off malarial infections, which means the majority of people bitten by infected mosquitoes either don't get the disease or develop only mild short-term symptoms.
- Supplements that can boost your immune system include: vitamins A, C and D, zinc, selenium, echinacea, olive leaf extract and astragalus root.[14] Be aware that these will not prevent malaria or its consequences.
-
3Avoid contaminated blood. The Plasmodium parasites that cause malaria primarily infect the liver, but also the red blood cells within blood. Consequently, people can also catch malaria by being exposed to contaminated (infected) blood.[15] Common modes of transmission due to contaminated blood include blood transfusions, sharing needles to inject drugs and childbirth (from an infected mother to her unborn child).
- Hemophiliacs and people who lose lots of blood from injuries are at higher risk of malaria from blood transfusions, particularly if they life in Africa or Asia.
- Malaria is not considered an STD (sexually transmitted disease), although there is a small chance of contracting it via sexual practices if the blood from one partner enters the bloodstream of another.
-
4Take preventative measures if traveling to at-risk areas. To prevent bites from Anopheles mosquitoes, avoid excessive exposure to the outdoors; wear long sleeves, pants, and cover as much skin as possible; wear insect repellant that contains N,N-diethyl-meta-toluamide (DEET) or picaridin); stay in well-screened or air-conditioned rooms; and sleep within bed nets treated with insecticide (such as permethrin). In addition, discuss taking anti-malarial medication with your doctor.
- Some drugs your doctor might suggest include chloroquine, atovaquone-proguanil (Malarone), artemether-lumefantrine (Coartem), mefloquine (Lariam), quinine, quinidine, doxycycline, clindamycin and artesunate (not currently licensed in the U.S.).[16]
Warnings
- Malaria should always be considered a potentially deadly disease. If you suspect that you have malaria, contact your doctor immediately.⧼thumbs_response⧽
- Malaria has symptoms that are very similar to a number of other more common conditions. It is very important that you tell your doctor if you have recently travelled to a malaria-endemic area, as otherwise malaria would be a very unlikely cause of these common symptoms, and may not be thought about early on.⧼thumbs_response⧽
References
- ↑ https://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/syc-20351184
- ↑ https://www.cdc.gov/parasites/malaria/index.html
- ↑ http://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/dxc-20167987
- ↑ http://www.cdc.gov/malaria/diagnosis_treatment/diagnosis.html
- ↑ http://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/dxc-20167987
- ↑ http://www.cdc.gov/malaria/diagnosis_treatment/diagnosis.html
- ↑ http://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/dxc-20167987
- ↑ http://www.cdc.gov/malaria/diagnosis_treatment/diagnosis.html
- ↑ http://www.medicalnewstoday.com/articles/150670.php
- ↑ http://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/dxc-20167987
- ↑ http://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/dxc-20167987
- ↑ http://www.cdc.gov/malaria/travelers/index.html
- ↑ https://www.who.int/en/news-room/fact-sheets/detail/malaria
- ↑ http://www.health.harvard.edu/staying-healthy/how-to-boost-your-immune-system
- ↑ http://www.mayoclinic.org/diseases-conditions/malaria/symptoms-causes/dxc-20167987
- ↑ https://www.cdc.gov/malaria/travelers/drugs.html
- ↑ http://www.mayoclinic.org/diseases-conditions/malaria/home/ovc-20167984
About This Article
To recognize malaria symptoms, watch for a high fever of at least 102 degrees Fahrenheit since this is one of the first signs of a malarial infection. You should also keep an eye out for other symptoms, such as shaking chills, headaches, muscle pains, vomiting, and diarrhea. If the malaria is advanced, you might notice yellowish skin and eyes as well as deep labored breathing. If you observe any of these symptoms, contact your doctor immediately so they can start treatment as soon as possible. For more information from our Medical co-author, including what preventative measures to take if you’re traveling to an area with a risk of malaria, read on!


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...