This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 24 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 159,689 times.
Research suggests that uterine fibroids are extremely common and often don't cause symptoms. However, some uterine fibroids cause long, heavy periods, pelvic pain, frequent urination, and constipation, so you likely want to prevent them.[1] Uterine fibroids (also called leiomyomas or myomas) are non-cancerous tumors that grow in your uterus, typically during your childbearing years. Experts aren't sure what causes fibroids, but it's possible the hormones progesterone and estrogen play a role in their development.[2] While there's no guarantee they'll work, certain lifestyle changes may help you limit your risk of fibroids.
Steps
Protecting Yourself Against Fibroids
-
1Exercise regularly. Uterine fibroids are hormonally mediated, much like tumors caused by breast cancer (although fibroids are not cancerous). Studies have shown that women who exercise regularly are less likely to develop fibroids.[3]
- Studies also suggest that the more physically active you are, the more that exercise will help you prevent fibroids. Women who exercised 7 or more hours per week were significantly less likely to develop fibroids over a period of several years than women who exercised two hours or less per week.[4]
- Research suggests that vigorous exercise is much more helpful in reducing your risk than light or moderate exercise. Vigorous exercise for 3 or more hours per week may reduce your risk of developing fibroids by 30-40%. (However, even light exercise is better than no exercise at all!)[5]
-
2Manage your weight. Research indicates that fibroids are more likely to occur in overweight or obese women (i.e., those with a BMI above the “normal” range). This may be because of the higher levels of estrogen in obese women.[6]
- Being overweight increases your risk of developing fibroids by about 10-20%.[7]
- Very obese women are two to three times more likely to develop fibroids than women within a normal BMI range.
- You can calculate your BMI using the Centers for Disease Control and Prevention’s website here. Or, you can use the following formulas: weight (kg) / [height (m)]2 or weight (lb) / [height (in)]2 x 703.
Advertisement -
3Drink green tea or use green tea extract. Some research has shown that green tea may help prevent the development of fibroids in rats. While it has not been confirmed in humans, green tea has numerous other health benefits, so it can’t hurt.[8]
-
4Consider changing your diet. Several studies suggest that consuming red meat is linked to an increased risk of developing fibroids. Eating green vegetables is associated with a decreased risk.[11]
- No evidence currently exists that suggests changing your diet will “prevent” fibroids. However, the health benefits of reducing red meat consumption and eating green vegetables are significant. Red meat consumption has been linked to many health issues, such as cardiovascular disease, cancer, and early mortality.[12] Green vegetables are excellent sources of vitamins, minerals, fiber, and antioxidants.[13]
- Eat foods high in Vitamin D, such as fatty fish (salmon, tuna, mackerel). Vitamin D may reduce your risk of developing fibroids by over 30%. Vitamin D can also shrink the size of existing fibroids.[14]
- Some research suggests that increasing dairy consumption — milk, cheese, ice cream, etc. — may reduce the risk of developing fibroids in African American women.[15]
-
5Recognize sham remedies. Some websites and “alternative” health sources suggest that remedies exist that can prevent or “cure” fibroids. Common remedies include enzymes, dietary changes, hormone creams, and homeopathy. There is no scientific evidence to support any of these treatments.[16]
-
6Understand that pregnancy and childbirth may have protective effects against developing uterine fibroids. Although researchers are not entirely certain why this is the case, women who have been pregnant have a lower risk of developing fibroids.[17]
- Pregnancy may also reduce the size of existing fibroids in some cases.[18] However, some fibroids may get bigger during pregnancy. Because fibroids are poorly understood, there is no way of knowing whether your fibroids will grow or not during pregnancy.
- Some research suggests that the protective effect of pregnancy is strongest during and immediately after pregnancy than for women whose pregnancies were farther in the past.[19]
Understanding Fibroids
-
1Know the risk factors of developing uterine fibroids. Fibroids are very common, especially in women who have reached childbearing age. Women who have not had children may be at higher risk of developing fibroids.[20]
- Your risk of developing fibroids increases as you age. Women between the age of 30 and menopause are the most commonly affected.[21]
- Having a family member, such as a sister, mother, or cousin, with uterine fibroids increases your risk of developing them.[22]
- Women of African descent appear more likely to develop fibroids, especially as they age. Some studies suggest that African American women are two to three times more likely to develop fibroids than white women. 80% of African American women develop fibroids by age 50, compared to 70% of white women. (Though, again, keep in mind that a large percentage of women who have fibroids do not experience any symptoms or problems related to the presence of the fibroids.)
- Women with a BMI (Body Mass Index) above the “normal” range” are more likely to develop fibroids.[23]
- Women who began menstruating at an early age (i.e., before 14) are at a higher risk of developing fibroids.[24]
-
2Recognize the symptoms of uterine fibroids. Many women who have fibroids do not know they have them. In many women, fibroids do not cause significant health problems. However, if you are experiencing any of the following symptoms, see your physician:[25]
- Heavy and/or prolonged menstrual bleeding
- Significant change in menstruation patterns (e.g., sharply increased pain, much heavier bleeding)
- Pelvic pain, or feelings of “heaviness” or “fullness” in the pelvic area
- Pain during sexual intercourse
- Frequent and/or difficult urination
- Constipation
- Backache
- Infertility or recurrent miscarriage
-
3Discuss treatment options with your doctor. If you do have fibroids, discuss treatment options with your doctor. In many cases, treatment is not necessary. However, in some cases, medication or surgical procedures may be necessary. The treatment your doctor recommends will vary depending on several factors, such as whether you wish to become pregnant in the future, your age, and the severity of the fibroids.[26]
- Drug therapy, such as hormonal birth control, may reduce heavy bleeding and pain. However, it may not prevent new fibroids or keep fibroids from growing.[27]
- Gonadotropin releasing hormone agonists (GnRHa) may be prescribed to shrink fibroids. The fibroids regrow rapidly once these medications are stopped, so they are primarily used pre-operatively to shrink fibroids in preparation for hysterectomy. They may have side effects including depression, decreased sex drive, insomnia, and joint pain, but many women tolerate these medications well.
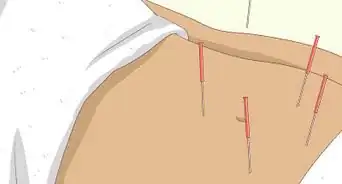
- Myomectomy (surgical removal of fibroids) may allow you to conceive children after the procedure. The risks depend on how severe the fibroids are. You may also be able to conceive after having MRI-guided ultrasound surgery, although this procedure is not widely available.[28]
- Other treatments for more severe fibroids may include endometrial ablation (surgical destruction of the uterus lining), uterine fibroid embolization (injection of plastic or gel particles into the blood vessels surrounding the fibroid), or hysterectomy (removal of the uterus). Hysterectomy is considered the last resort when other treatments and procedures have not worked. Women cannot have children after some of these procedures.[29]
- Women who conceive after undergoing embolization may experience complications with their pregnancies, so this method is not recommended for women who may become pregnant in the future.
Warnings
- Rapidly growing fibroids could actually be a sign of a rare cancer of the uterus (leiomyosarcoma) and should be investigated by a physician.⧼thumbs_response⧽
- There may be no way to prevent fibroids. Following recommendations to prevent fibroids may reduce your chances of having them, but it will not guarantee that you will not develop them.⧼thumbs_response⧽
- Fibroids may be surgically removed if they cause problems; however, they tend to grow back. The only way to ensure fibroids do not regrow is to undergo a hysterectomy. A hysterectomy also has complications and long-term effects of its own. The procedure needs to be discussed thoroughly with your doctor.[31]⧼thumbs_response⧽
References
- ↑ https://www.womenshealth.gov/a-z-topics/uterine-fibroids
- ↑ https://www.womenshealth.gov/a-z-topics/uterine-fibroids
- ↑ http://aje.oxfordjournals.org/content/165/2/157.full
- ↑ http://aje.oxfordjournals.org/content/165/2/157.full
- ↑ http://www.niehs.nih.gov/research/atniehs/labs/assets/docs/k_p/october_2004_508.pdf
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/1802214
- ↑ http://www.niehs.nih.gov/research/atniehs/labs/assets/docs/k_p/october_2004_508.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3742155/
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/23950663
- ↑ https://my.clevelandclinic.org/health/articles/15496-caffeine-how-to-hack-it-and-how-to-quit-it
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7908561/
- ↑ http://www.health.harvard.edu/staying-healthy/cutting-red-meat-for-a-longer-life
- ↑ http://www2.ca.uky.edu/agc/pubs/fcs3/fcs3567/fcs3567.pdf
- ↑ http://www.nih.gov/news/health/mar2012/nichd-01.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7908561/
- ↑ http://www.mayoclinic.org/diseases-conditions/uterine-fibroids/basics/alternative-medicine/con-20037901
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/9757871
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2927730/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1847588/
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Uterine_Fibroids
- ↑ https://medlineplus.gov/ency/article/000914.htm
- ↑ https://medlineplus.gov/ency/article/000914.htm
- ↑ https://nwhn.org/fibroids
- ↑ http://www.niehs.nih.gov/research/atniehs/labs/assets/docs/k_p/october_2004_508.pdf
- ↑ https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids
- ↑ https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids
- ↑ https://www.acog.org/womens-health/faqs/uterine-fibroids
- ↑ https://www.acog.org/womens-health/faqs/uterine-fibroids
- ↑ https://medlineplus.gov/ency/article/000914.htm
- ↑ https://www.health.ny.gov/community/adults/women/uterine_fibroids/
- ↑ https://www.womenshealth.gov/a-z-topics/uterine-fibroids









-Step-3.webp)





















-Step-3.webp)




































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...