This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 69,681 times.
You may not be able to eliminate your risk of breast cancer altogether, but even a few simple lifestyle changes can help decrease your risk! Our how-to guide will show you a number of different ways you can help you manage your risk factors, starting today.
Steps
Controlling Your Risk Factors
-
1Limit your alcohol intake. The more you drink, the more you increase your risk of breast cancer.[1]
- If you choose to drink alcohol, including wine, beer, or liquor, take steps to limit your consumption to no more than one drink per day.
- For every drink you have each day, statistics show that you are increasing your risk by 10% to 12% over those that do not drink.[2]
- The reasons behind the increased odds of breast cancer associated with all forms of alcohol are not clear, but there has been an association between blood alcohol levels and changes in the amounts of estrogens and other hormones that circulate in the blood.
-
2Quit smoking. If you are a smoker, then take steps to quit. If you are a non-smoker, then don’t ever start.[3]
- Smoking has been linked to many forms of cancer and recent evidence is now suggesting it also increases the risk of developing breast cancer.
- The research found that you have a 24% higher risk of getting breast cancer if you smoke.
- Former smokers have a 13% higher risk of getting cancer compared to those that never smoked.
- Another study supports those numbers and adds that women who started smoking at an early age have a 12% increase in their odds of getting breast cancer. Women that started smoking before their first pregnancy have a 21% increase in risk.
- This may all sound like risk factors that you can’t control based on your smoking history, but you can control what you do now to decrease your odds. If you are a smoker, take steps to quit.
Advertisement -
3Maintain a healthy weight. Being overweight has been shown to increase your risk of breast cancer.[4]
- The odds of breast cancer are even greater if the weight gain, or obesity, developed after menopause.
- Women that gained their weight after menopause have a 30% to 60% higher risk of developing breast cancer.[5]
- Oddly, women that were overweight or obese before menopause have a 20% to 40% less likely to develop breast cancer compared to women of healthy weight.
- The reasons behind the weight changes and timing are not entirely clear but are thought to be related to hormonal fluctuations.
-
4Be physically active. There are many benefits to being physically active, one of which is tied to reducing your risk of breast cancer.[6]
- The general guidelines for physical activity include 150 minutes each week of moderate aerobic activity.
- If you are already exercising, the suggested amount of vigorous activity to reduce your risk is 75 minutes each week of aerobic activity in addition to strength training at least twice weekly.
- Start exercising now. Some research suggests that women that have maintained an inactive lifestyle for many years may be at greater risk.[7]
-
5Breast-feed your baby. The longer you breast-feed, the more you reduce your risk.[8]
- While the reduction in risk is relatively small, it is still a way you can improve your odds against developing breast cancer.[9]
- You can reduce your risk by 4.3% for every 12 months you breast-feed. That includes one child or several.
-
6Limit hormone therapy. There is an increase in the risk of breast cancer in women that take hormone therapy for the symptoms associated with menopause.[10]
- Research suggests that taking combination hormone therapy, meaning you are taking both an estrogen product and a progesterone product or that both types are contained in the same pill, increases your risk of breast cancer.[11]
- Work done shows that the increase in risk also includes more cases of invasive breast cancer leading to more cancer deaths in women that take combination hormone therapy, even for a short time.
- The other type of hormone therapy contains estrogen only. This form also increases your risk but only if you take the hormone therapy for an extended amount of time, such as 10 years or more. If you do not have a uterus and take estrogen alone, it may actually reduce your chances of breast cancer.
- The good news is that once you stop taking hormone therapy, your risks drop back to normal in about three to five years.
- If you feel you need hormone therapy to control menopausal symptoms, talk to your doctor about reducing your dose. This is one way to limit your exposure to hormone therapy.
-
7Avoid exposure to radiation. Exposure to high doses of radiation to the chest area has been linked to an increase in the incidence of breast cancer.[12]
- Some diagnostic testing equipment, such as computerized tomography, known as CT scans, use high levels of radiation.
- While diagnostic testing is critical in determining the source of medical problems, talk to your doctor about other methods that might work as well as CT scans in order to limit the exposure of radiation to your chest area.
- Be sure to wear the recommended protective equipment if you work in an area that involves radiation treatments.
- Some jobs require exposure to environmental pollutants such as chemical fumes and gasoline exhaust that can also be dangerous. Be sure to understand the proper steps to take in order to keep yourself protected from exposure to environmental pollutants.
-
8Eat a healthy diet. There are many benefits to eating a healthy diet, including controlling your weight which is a way to reduce your risk.
- A diet that is rich in fruits and vegetables may be helpful in preventing breast cancer although study results are inconclusive in showing a clear protective effect.
- A slight improvement in breast cancer survival has been noted with a consistent diet that is considered low-fat.
- The benefit of the low-fat diet was reported as significant in the survival of women that were already diagnosed with breast cancer.[13]
- The dietary changes included steps such as eliminating butter, margarine, cream, oils included in salad dressings, and fatty meats such as sausages.
Identifying Risk Factors Beyond Your Control
-
1Review your family history. Genetics play a significant part in your risk of developing breast cancer.
- Estimates suggest that between 5% and 10% of cancers develop due to genetics.
- Even though the family history is important, the majority of women that develop breast cancer do not have a family history at all.
- Depending on your personal family history, your doctor may recommend that you have the blood test to determine if you are carrying the identified genes.
- The most common genes that have been identified as contributing to breast cancer are called BRCA1 and BRCA2. 45-65% percent of people who inherent these genes develop breast cancer prior to age 70.
- Ask for a referral. If your doctor is not able to perform the genetic testing, ask your doctor for a referral to a geneticist that can review your family history and make specific recommendations regarding the possible need for the genetic testing.
-
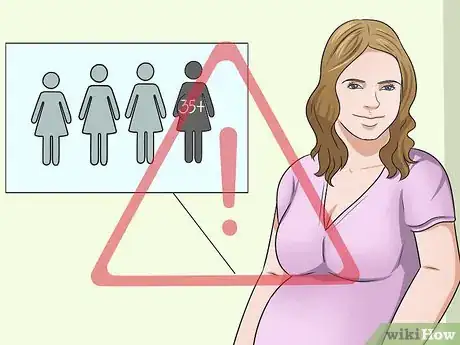
2Recognize age-related factors. Several variables increase the odds of developing breast cancer that are related to age.
- First of all, just aging is considered a risk factor. The older you get, the greater the chance of developing breast cancer.
- Beginning your period before 12 years of age is a risk factor for breast cancer later in life.
- Experiencing menopause at an older that average age is considered a risk factor. The average for menopause is about 51 years of age.
-
3Consider pregnancy factors. Some relationships have been established that may increase your risk based on pregnancy.
- Women that have never been pregnant are considered to be at an increased risk.
- Delivering your first child after age 35 is considered to increase your risk of breast cancer.
-
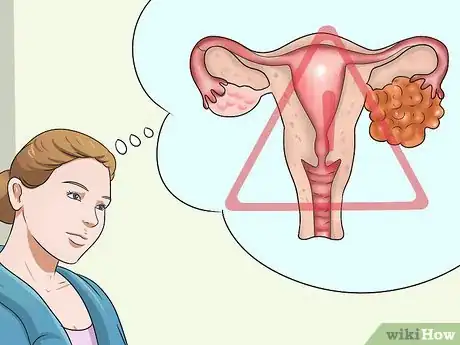
4Take into account additional factors. Breast cancer is a complex disease that make it impossible to predict those that will or will not develop it, even when all risk factors are considered. Additional factors that have been identified as contributing to the chance of getting breast cancer include the following:
- A personal history of breast cancer.
- Radiation treatment or exposure to the chest area as a child or young adult.
- Having dense breast tissue. A certain kind of hormonal replacement therapy (Duavee) may decrease this risk.[14]
- A personal history of ovarian cancer.
- Getting pregnant for the first time after the age of 30.
- Never getting pregnant.
- Taking a drug called DES, or diethylstilbestrol, which was prescribed to prevent miscarriage during the years between 1940 and 1971.
- Being exposed in the uterus if your mother took the same drug while pregnant with you.
Monitoring Changes in Your Breasts
-
1Detect changes in your breast. Early awareness and rapid treatment are key variables in improving your odds of a total recovery should you develop breast cancer. Understand the signs and symptoms in order to monitor yourself for changes. The signs and symptoms of breast cancer include the following:
- A lump or thickening that you can feel, and it feels different than the tissue around that area.
- The lump or hardened area of tissue can be anywhere in your breast, including deep within the tissue and up against your chest wall and in the area under your arm.[15]
- Bloody drainage or discharge from your nipple area.
- Change in the size of your breast.
- Change in the shape or appearance of your breast.
- Dimpling of the skin of your breast.
- Redness or a pitted appearance of the skin anywhere on your breast, similar to the skin of an orange.
- Swelling, warmth to the touch, or a redness or darkening of the breast tissue.[16]
- A painful spot or area that persists.
- A change in your nipple including an inverted nipple.
- Peeling, flaking, or scaling, of the areola, which is the darker colored area that immediately surrounds your nipple, or anywhere on your breast.
-
2Examine your own breasts. Knowing what is normal for you is important in detecting changes early.[17]
- The effectiveness of breast self-exams have been studied. The results show no difference in the early detection of breast cancer identified in women that performed breast self-exams as compared to those who did not.
- The research also showed that more false alarms leading to biopsies and additional testing occurred in the group of women that performed the breast self-exams.
- It is very important for you to know what is normal for you. Many women still choose to follow the recommendations provided to perform breast self-exams. Self-awareness by the established steps for self-exam, use of your own method, or routine observations of your breast and nipple tissue, is important in detecting early changes that may be significant.
- Anything that changes from what is normal for you warrants medical attention as soon as possible.
- Review the recommended method for breast self-exam. Follow those guidelines or develop your own method to routinely monitor for changes using a schedule that you can keep up with.
- If you choose to perform breast self-exams following published guidelines, then know the most recent recommendations for how to do it.[18]
-
3Start by examining your breast tissue by touch. Keep in mind that you should perform the exam lying down as opposed to standing.[19]
- The breast tissue tends to spread out more evenly, allowing you to perform a more thorough exam.
- Position yourself flat on your back and place your right arm beneath your head.
- Use the pads of the three middle fingers of your left hand to examine your right breast.
- Use circular motions, about the size of a dime, and overlap your circles to cover all the tissue of your right breast.
- Follow an up and down pattern while incorporating the circular motions.
- Use lighter pressure to feel the tissue closest to the surface, medium pressure allows you to feel a little deeper, and firm pressure helps you feel the tissue closest to the chest wall and the ribs.
- Use the dime-size circular motions with each of the three levels of pressure in a methodical up and down pattern to cover the entire breast. Examine tissue up to the neck and collar bone area, include the middle part of your chest where your sternum or breastbone is located, and include your underarm areas.
- Switch arms and hands, and repeat to examine your other breast.
- It is normal to feel a ridge along the lower curved area for each breast. If you are unsure of something you are feeling, check to see if the same thing is felt at the exact same place on the other breast. If you feel the same thing in the same place on both sides, then it is probably perfectly normal.
-
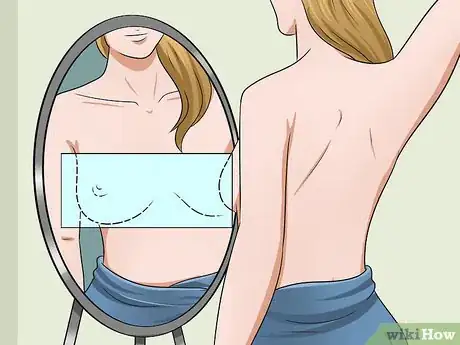
4Continue in front of a mirror. Stand in front of a mirror in an area with good lighting and press down on your hips.[20]
- Pressing down on your hips alters the position of your chest wall and helps to make any breast changes more obvious.
- Look for any changes in size, shape, or contour of your breasts. It is not uncommon for one breast to consistently be slightly larger than the other.
- Next look for changes in skin color or texture, such as redness, dimpling, and scaly, flaky skin, especially around the nipples.
- Slightly raise one arm and feel under your arm for any abnormalities, lumps, or changes. Raising your arm only slightly helps to make any changes more noticeable to touch and gentle pressure.
- Do breast self-exams with implants. It is possible to effectively perform breast self-exams with implants.
- Talk to your surgeon so you know where the edges of your implants are located.
-
5Notice changes in lumpiness. Breast tissue is naturally lumpy.[21]
- Lumpy breasts are usually nothing that indicates a problem, especially if the consistency of the lumpy feeling is the same throughout the breast and both breasts feel the same way.
- If you notice a lump or hardened area that feels different than the rest of the lumpiness in your breast tissue, contact your doctor as soon as possible.
-
6Have any new lump examined. Many women have developed unusual lumps in their breast tissue in their past.[22]
- Most cases resulted in a thorough exam that resulted in finding an actual lump but it was benign, or was not cancer.
- If you had a lump in the past and it turned out to be benign, do not assume that this new one will also be benign. See your doctor for an examination as soon as possible.
-
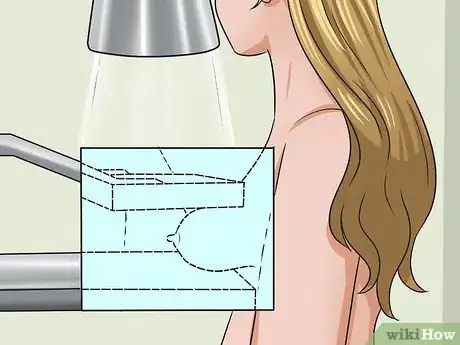
7Watch for nipple discharge. Liquid that leaks from your breast is alarming but is not usually a sign of anything serious.[23]
- Squeezing your nipple can result in some leakage. This is almost always completely normal.
- See your doctor if your nipple is leaking liquid without squeezing.
- If the drainage is occurring from only one breast, have your doctor examine you.
- Drainage that is bloody or clear warrants seeing your doctor for evaluation.
- There are reasons other than cancer that can cause your nipples to leak, most often being the results of an infection. Any leakage from your nipple should be examined by your doctor.
-
8Seek immediate medical attention. See your doctor immediately if you notice any potential symptoms in your breast.
- Even if you have had a recent exam and/or a recent mammogram, any changes you notice should be examined by your doctor immediately.
- Breast cancer cells divide more rapidly than the cells in normal tissue. Once you become aware of an abnormal area or change in your breast tissue, seek medical attention as soon as possible.
Participating in Recommended Medical Screening
-
1Have a mammogram. Having a mammogram is an essential part of early detection.[24]
- According to the American Cancer Society, the scientific evidence supporting the use of mammography to detect early breast cancer is stronger than ever.
- A mammogram is not 100% perfect. Even a mammogram can miss small growths that are cancerous and the test may identify some areas that turn out not to be cancerous.
- The American Cancer Society recommends that women 40 years of age and older have a yearly clinical breast exam by a doctor and a yearly mammogram.
- This recommendation holds for the duration of life provided there are no health conditions that place the person at risk or make it necessary to perform mammograms on a case-by-case basis.
- Examples of some medical conditions that might need special consideration include women with congestive heart failure, end-stage renal disease, chronic obstructive pulmonary disease, and moderate to severe dementia.
- Women in their 20’s and 30’s are recommended to undergo routine clinical breast exams. They rarely undergo mammograms unless advised to do so by their doctor.
- Depending on your personal risk factors, your doctor may advise that you have more frequent clinical breast exams and mammograms.
-
2Have a clinical breast exam as recommended. Depending on your age and risk factors, you will likely be advised to have a clinical breast exam every one to three years.[25]
- A clinical breast exam is done routinely during your regularly scheduled gynecology appointments.
- Your doctor or other qualified healthcare professional that is performing the clinical breast exam will visually examine your breast for abnormalities in size, shape, condition of the breast tissue, and the nipple area.
- The doctor will then use the tips of his or her fingers to gently feel all around along the entire area of your breasts.
- The doctor will be checking for any abnormalities within your breast tissue such as lumps or hardened areas. If any lumps or hardened areas are located, the doctor will further press on your breasts to determine if they are connected to deeper tissues.
- The areas under both arms will be examined in the same manner.
- During the clinical breast exam, ask questions so you can improve your ability to perform a similar self-exam at home.
-
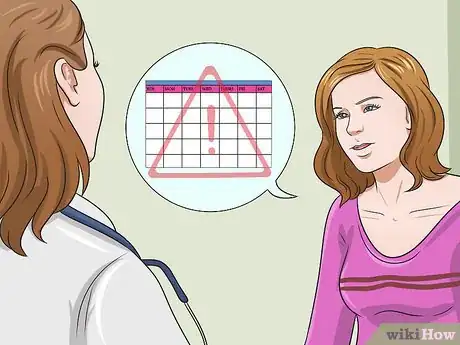
3Ask your doctor about your lifetime risk assessment. Some women with combined and more serious risk factors may need frequent and more intense screening.[26]
- Talk to your doctor about your lifetime risk and recommendations. As new scientific information becomes available, the associated recommendations sometimes change.
- The current, 2014, recommendations include the use of both mammogram and MRI studies to be done each year in women that are considered to have a lifetime risk of greater than 15%.
- Many variables go into the assessment to determine your lifetime risk. Talk to your doctor to be sure you are properly evaluated and comply with the screening procedures recommended.
-
4Have an MRI if recommended. An MRI, or magnetic resonance imaging, is a tool that identifies abnormalities in the breast that may have been missed in a mammogram.[27]
- Only women determined to have a higher lifetime risk are recommended to undergo both an MRI and a mammogram. You still need the mammogram because it can detect abnormal areas that the MRI screening might miss.
- A breast MRI is done by lying face down on a platform in a standard MRI tube or tunnel-like device.
- The platform that you lie on contains special equipment that allows your breast tissue to be exposed through openings as opposed to compressing the tissue which happens with the mammogram. The platform has the sensors needed to perform the imaging study.
- It usually takes about an hour to perform a breast MRI. It is important that you remain perfectly still during the procedure.
- A breast MRI requires an injection of a contrast material injected through a catheter into a vein of the arm just before beginning the procedure.
- Breast MRI is expensive so it may be helpful to go to a doctor or clinic that is accustomed to working with moderate to high risk women so they can take the best approach with your insurance company or third party payer.
References
- ↑ http://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/breast-cancer-prevention/art-20044676
- ↑ http://www.cancer.org/cancer/news/expertvoices/post/2013/06/26/does-drinking-alcohol-increase-the-risk-of-cancer.aspx
- ↑ http://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/breast-cancer-prevention/art-20044676
- ↑ http://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/breast-cancer-prevention/art-20044676
- ↑ http://ww5.komen.org/BreastCancer/OverweightWeightGain.html
- ↑ http://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/breast-cancer-prevention/art-20044676
- ↑ https://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000830.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000830.htm
- ↑ http://www.cancer.org/cancer/news/expertvoices/post/2013/05/07/can-breastfeeding-lower-breast-cancer-risk.aspx
- ↑ http://www.cancer.org/cancer/news/expertvoices/post/2013/06/26/does-drinking-alcohol-increase-the-risk-of-cancer.aspx
- ↑ http://www.breastcancer.org/risk/factors/hrt
- ↑ http://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/breast-cancer-prevention/art-20044676
- ↑ http://www.medscape.com/viewarticle/836606
- ↑ https://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000830.htm
- ↑ http://ww5.komen.org/BreastCancer/WarningSigns.html
- ↑ http://ww5.komen.org/BreastCancer/WarningSigns.html
- ↑ http://ww5.komen.org/BreastCancer/BreastSelfExam.html
- ↑ http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf
- ↑ http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf
- ↑ http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf
- ↑ http://ww5.komen.org/BreastCancer/WarningSigns.html
- ↑ http://ww5.komen.org/BreastCancer/WarningSigns.html
- ↑ http://ww5.komen.org/BreastCancer/WarningSigns.html
- ↑ http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf
- ↑ http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf
- ↑ http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf
- ↑ http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf
About This Article
To prevent breast cancer, try to limit your alcohol intake to no more than 1 drink per day since the more you drink, the higher your risk of breast cancer is. You should also eat a healthy diet and exercise regularly so you maintain a healthy weight, which can reduce your risk of developing breast cancer. Also, if you smoke, try to take steps to quit since smoking can significantly increase your chances of getting breast cancer. For more advice from our Medical co-author, like how to monitor changes in your breasts, scroll down!








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...