This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 18 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 13,093 times.
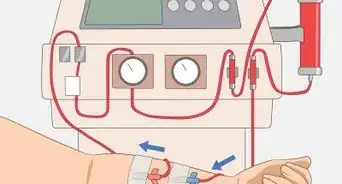
If your phosphate levels are too high, you may be a little worried. Typically, this condition arises when your kidneys aren't working quite right. In particular, high blood phosphorous levels can be a sign of extensive kidney damage.[1] Your doctor may want you to lower your phosphate levels, which you can do by watching your dietary intake and swapping out certain foods. Phosphate binders can also help. These medications stop you from absorbing as much phosphate from your diet.
Steps
Watching Your Dietary Intake
-
1Have your phosphate levels checked by your doctor. Before you start making changes to your diet, you should know where your levels are. Your body needs phosphate to build strong bones and to assist with muscle movement and nerve signaling. If you start removing it from your diet without knowing where your levels are, you could risk lowering your phosphate too much.[2]
- Your doctor will do a blood test to check your phosphate levels. The normal range is 2.4 to 4.1 mg/dL.
-
2Talk to your doctor and a dietician to determine a safe diet for you. Ask your doctor for a recommendation for a dietician. A dietician who specializes in low-phosphate diets can help you better navigate your food choices.[3]
- How much phosphate you can ingest depends on your blood tests and your kidney function.
Advertisement -
3Read labels to check for phosphate or phosphoric acid. Many processed foods have added phosphate, so you should always check the ingredients list. Foods like cake mixes, ham, sauce mixes, and even sodas can have added phosphate in them.[4]
- Look for any ingredient that starts with "pho." Names of phosphates can include the following:
- Dicalcium phosphate
- Disodium phosphate
- Monosodium phosphate
- Phosphoric acid
- Sodium hexameta-phosphate
- Trisodium phosphate
- Sodium tripolyphosphate
- Tetrasodium pyrophosphate[5]
- Avoid these foods in your diet.
- Look for any ingredient that starts with "pho." Names of phosphates can include the following:
-
4Avoid fast food and processed foods completely. Fast foods are highly processed, and they often have added phosphates. It's best to skip these foods altogether to keep the extra phosphates out of your diet.[6]
- If there's a fast food you really want to eat, check out the ingredient list online. If it's not online, contact the company to ask for the ingredients.
-
5Eat fewer than 5 eggs a week. Eggs are a complete protein, but they do contain some phosphate. You can still eat them, but you should limit your intake. Don't consume more than 4 eggs each week.[7]
- Don't eat more than 1 egg a day.
-
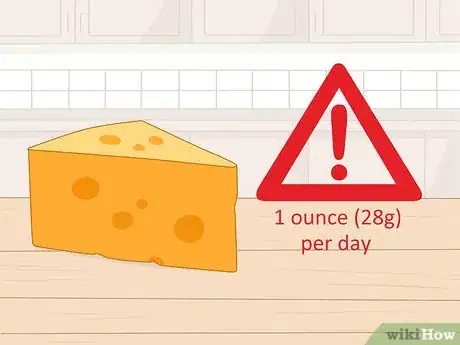
6Limit cheese to 1 ounce (28 g) per day. While some cheeses have less phosphate in them, such as cream cheese, it's best to limit your intake anyway. Don't eat more than 1 ounce (28 g) of cheese in a day.
- 1 ounce (28 g) of cheese is about the size of 2 standard dice.
-
7Lower your other dairy to a single serving a day. For instance, you can drink 1 cup (240 mL) of milk a day. Alternatively, you can replace 1⁄2 cup (120 mL) of that serving with 1 yogurt, 2 small scoops of ice cream, or a small bowl of rice pudding.
- Some doctors and dieticians may recommend that you skip dairy altogether. It's always best to consult with your doctor before deciding on your dietary choices.
Swapping out Foods
-
1Choose unenriched rice milk over dairy milk and yogurt. Most dairy products are high in phosphate, including milk, yogurt, and pudding. Non-dairy creamers, soy milk, and even enriched rice milk contain higher concentrations of phosphates than unenriched rice milk.[8]
- Similarly, instead of ice cream, try sherbet, sorbet, or fruit-based popsicles.
-
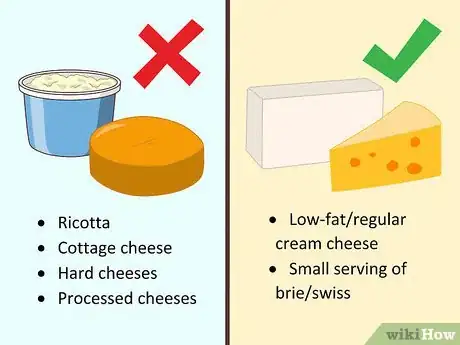
2Opt for cream cheese, brie, or Swiss over other cheeses. Ricotta, cottage cheese, hard cheeses, and processed cheeses are all higher in phosphate. Instead, choose low-fat or regular cream cheese, or a small serving of brie or Swiss, which have lower levels of phosphates.[9]
- You should also avoid cheese spreads.
-
3Pick lemon-lime soda, root beer, or ginger ale over dark sodas.[10] Most dark sodas or "pepper"-type sodas have phosphates in them. Lighter sodas are less likely to have phosphates in them, making them a better choice. Always read the label to check for phosphates, though.[11]
- An even better drink option is plain water or tea.
-
4Choose fruit candies over chocolate or caramels. Chocolate is high in phosphates, so limiting it or completely cutting it out is recommended. In fact, anything that contains chocolate or cocoa is generally off limits if you're trying to limit your phosphate intake. If you feel like you need a little chocolate, opt for dark varieties that are a least 70% cacao, and always have it in moderation.[12]
- If you're craving chocolate, ask your dietitian if you can have a chocolate bar that just as a thin coating of chocolate around other ingredients.
-
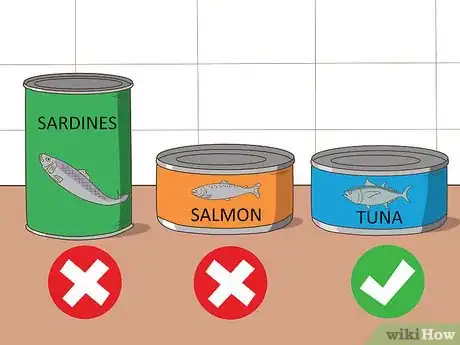
5Opt for fresh or boneless canned fish over fish with bones. Canned fish with the bones still in it, such as salmon or sardines, are higher in phosphates. Canned fish without bones, such as tuna, is lower in phosphates.[13]
- Fresh or frozen boneless fish is also a good option.
-
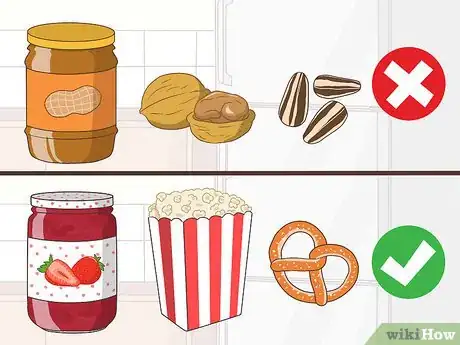
6Switch nuts, seeds, and nut butters out for popcorn, pretzels, and jams. If you're looking for a snack, popcorn or pretzels are a good, crunchy option you should be able to tolerate. If you want a spread, opt for jam, jelly, or honey.[14]
- Corn snacks, rice cakes, or crunchy breadsticks are also good options.[15]
-
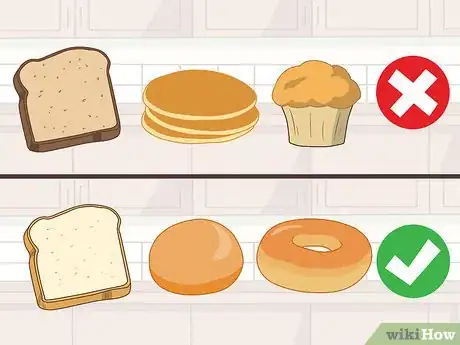
7Go for white breads and rolls instead of whole wheat or quick breads. Whole grains tend to have more phosphate than refined grains, so opt for white bread over whole wheat. Also, choose yeast breads like rolls, bagels, or English muffins over quick breads like cornbread, pancakes, or muffins.[16]
- Check the bread label for phosphate additives.
-
8Choose green beans or green peas over peas or lentils. Dried peas, beans, and lentil have more phosphate. That includes garbanzo beans, lentils, lima beans, black beans, navy beans, pinto beans, and black-eyed peas.[17]
- Canned, fresh, or frozen peas or green beans are fine, as long as they don't have added phosphates.
-
9Skip lunch meats and hot dogs in favor of fresher meat. Processed meats, like other processed foods, often have added phosphates. Instead, pick fresh or frozen meat like pork chops, ground beef, chicken, or fish.[18]
- Skip meats like ham and bologna. You may be able to eat uncured bacon, but check the label for phosphates.
Using Phosphate Binders
-
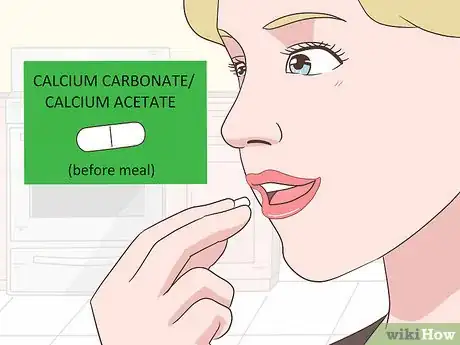
1Chew calcium carbonate or calcium acetate before you eat. Taking a 500-milligram tablet of calcium carbonate before you eat can lower how much phosphate you absorb from your diet. Chew the tablet thoroughly and swallow right before you eat your meal.[19]
- Calcium carbonate is the active ingredient in a number of antacids, such as Tums or Rolaids. It is relatively safe unless your calcium is already high, which can happen if you are having kidney issues. Always talk to your doctor before beginning a medication regimen.
- This medication can cause side effects like upset stomach, dry mouth, vomiting, and diarrhea.[20]
- You can also try a combination of calcium carbonate and magnesium carbonate. This combination has lower calcium levels, though it still contains calcium.
-
2Try Sevelamer hydrochloride for a non-calcium option. If you can't take a calcium-based option, then this tablet will likely be your doctor's next recommendation. Typically, you'll take either 1-2 800 milligram tablets or 2-4 400 milligram tablets before each meal.[21]
- Eat 2-3 bites of your meal, then swallow this medication.[22]
- This medication can cause digestive problems, such as trouble swallowing, indigestion, diarrhea, and constipation.
- If you're having stomach pains after getting on this medication, talk to your doctor about what you should do.
-
3Take lanthanum carbonate for another calcium-free option. Take this medication as a chewable tablet or a powder you sprinkle on your food. You can eat it with your meal or directly after.[23] The tablets come in 500 milligram, 700 milligram, and 1,000 milligram dosages.[24] The powder comes in 700 milligram or 1,000 milligram sachets of powder.[25]
- To use the powder, sprinkle it on a little applesauce or another soft food, and eat it all immediately. It doesn't dissolve in liquid.
- Take thyroid medications and antacids at least 2 hours before or 2 hours after taking this medication. Take antibiotics 1 hour before or 4 hours after taking this medication.
- This medication can also cause digestive problems, such as constipation, diarrhea, nausea, and vomiting. Talk to your doctor if you have these symptoms.
-
4Use sevelamer carbonate in place of calcium carbonate. This medication comes in a chewable tablet or powder form. Typically, you start on 800 milligrams per meal, though your doctor may also start you out at 1.6 grams (0.06 oz).[26] Chew the tablet with your meal, or stir the powder into 2 fluid ounces (59 mL) of water to drink with your meal.[27]
- The side effects of this medication include vomiting, nausea, diarrhea, and other digestive problems. Discuss these side effects with your doctor.
Warnings
- Keeping your phosphate levels in check is only a part of managing kidney disease. Other factors to talk to your doctor about include blood pressure, CMP, creatinine clearance, and blood urea nitrogen.⧼thumbs_response⧽
References
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf
- ↑ https://medlineplus.gov/ency/article/003478.htm
- ↑ https://www.kidney.org/atoz/content/phosphorus
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf
- ↑ https://www.kidney.org/atoz/content/phosphorus
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.kidney.org/atoz/content/phosphorus
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.mayoclinic.org/food-and-nutrition/expert-answers/faq-20058408
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf
- ↑ https://medlineplus.gov/druginfo/meds/a601032.html
- ↑ https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=aa991f60-7c13-49ec-862b-47cca4db3c44
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf
- ↑ https://www.fda.gov/downloads/Drugs/DrugSafety/UCM271798.pdf
- ↑ https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021468s016lbl.pdf
- ↑ https://www.medicines.org.uk/emc/product/4166/smpc
- ↑ https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e6328460-a57b-450b-a48c-6dcd4b476360
- ↑ https://www.ouh.nhs.uk/oku/patient-advice/documents/phosphate-diet.pdf


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...