This article was co-authored by Timothy Sherman, RN. Timothy Sherman is a Registered Nurse (RN) based in Austin, Texas and affiliated with St. David's HealthCare. With over seven years of nursing experience, Timothy specializes in working with adults in a general medical/surgical setting, chemotherapy, and with biotherapy administration. He has also instructed Essentials of Medical Terminology and Anatomy and Physiology for Medical Assistants at Austin Community College. He received his BS in Nursing from Wichita State University in 2012.
There are 18 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 41,583 times.
Otitis media is the medical term for an ear infection in your middle ear, which is the space behind your eardrum. When healthy, the middle ear is filled with air, and it connects to the nasopharynx (the back of your nose/top of your throat) through the Eustachian tube. You or your child can develop ear infections in this area, causing it to fill with fluid and resulting in pain. You need to be able to recognize the symptoms in your children as well as in yourself, and you need to know when you should see a doctor.
Steps
Recognizing Symptoms in Adults and Teens
-
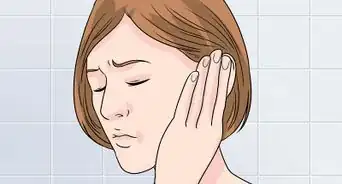
1Pay attention to pain that develops in your ear. If you've developed an earache, that can be a sign that you have otitis media. The pain can be a constant, dull ache, accompanied by throbbing, or it can be sharp, stabbing pains that come and go, either alone or in combination with a duller ache.[1]
- The pain results from the fact that you have infected fluid in your middle ear, which presses on the eardrum.[2]
- This pain may also spread. You may experience a headache or neck pain, for instance.
-
2Monitor any mild hearing loss that occurs. You may also begin to temporarily lose some of your hearing. When fluid builds up behind the eardrums, it can slow down the signals that go to your brain as they pass through the tiny bones of the inner ear; therefore, you may experience some hearing loss.[3]
- Some people also hear a ringing or buzzing in their ears that comes and goes.
Advertisement -
3Watch for fluid drainage. When your ear is infected, you may also have fluid drainage. Pay attention if pus or other fluids drain from your hurting ear. The fluid may be brown, yellow, or white. This fluid means your eardrum has ruptured, and you need to see a doctor.[4]
-
4Note complementary symptoms. Sometimes, ear infections develop alongside other symptoms, such as a runny nose or sore throat. If you have these symptoms in conjunction with an earache, talk to your doctor about the possibility of having an ear infection.
Watching for Signs in Children and Babies
-
1Check for signs of ear pain. Children tend to have acute pain with ear infections. In younger kids, they may not be able to express that pain; however, you can watch for excessive crying, particularly when the child lays down, as well as pulling or tugging on their ears.[5]
- They may also be more irritable or have difficulty sleeping.
-
2Watch for decreased interest in eating. This symptom is most prevalent in babies that are breast or bottle feeding. As they swallow, it causes more pain in the ear, due to a change in pressure; therefore, the child doesn't want to eat as much because of the pain.[6]
-
3Look for difficulty hearing. Just like in adults, otitis media can cause temporary hearing loss in children. Pay attention to see if your kid doesn't seem to be hearing as well as normal, such as not being able to answer questions well or repeatedly asking "What?" when you are talking.[7]
- In babies, watch to see if they respond to soft sounds as well as they normally do.
-
4Check for a fever. Often, children with this condition will run a fever. Check your child's temperature if you suspect they have an ear infection. A child with an ear infection can run a relatively high fever, from 100.4 to 104°F (38 to 40°C).[8]
-
5Notice problems with your child's balance. Another symptom of a middle ear infection is the child having problems with balance. Because the ear regulates balance, an infection can cause a child's balance to be off. Pay attention if your child suddenly has more trouble walking or staying upright.[9]
- Balance problems are more likely to be a symptom for kids than adults, but you should take note if you are having balance problems along with other symptoms.
-
6Look for nausea and vomiting. This condition can also cause your child to be nauseated, due to the vertigo (lack of balance) caused by the ear infection. It can also lead to vomiting. Look for these symptoms along with other signs, such as pain or mild hearing loss.[10]
-
7Realize symptoms may not be dramatic. Sometimes, this condition doesn't exhibit many symptoms. In fact, the main symptom may be mild hearing loss, which your child or you may not even notice. It may exhibit as the child not paying as much attention in school, for instance, because they can't hear as well.[11]
- Other kids may notice their ear feeling "full," or the ear may pop more often.
-
8Pay attention to drainage. Once again, drainage is usually a sign that the eardrum has ruptured. Do not be fooled by the pain relief that often results from an eardrum rupturing.[12] The pressure on the eardrum has been released, but the infection has made a serious progression. You definitely need to go to the doctor as soon as possible if you see yellow, brown, or white fluid draining from the ear.[13]
Knowing When to Head to the Doctor
-
1Call a doctor depending on how long symptoms last. Pay attention to how long the symptoms are present. You should particularly pay attention if the symptoms appear after you or your child has had another infection, such as a cold, since that makes you more susceptible to ear infections, particularly in children.[14]
- For babies under half a year old, see a doctor when symptoms appear.
- For children and adults who've had symptoms last more than 24 hours, call your doctor for advice.
-
2Go to the doctor if your temperature climbs. If you or your child have been running a fever, it's time to talk to the doctor. A fever is a sign of infection, and you or your child may need a round of antibiotics to help fight the infection.[15]
- If your child's temperature goes over 100.4°F (38°C), it's time to go to the doctor.
-
3Talk to your doctor if ear pain is severe. Severe ear pain indicates it's time to get advice from your doctor. It could be an indication the infection is worsening or spreading. Call your doctor if you or your child's pain is particularly severe.[16]
- With your child, pay attention to see if they are in more pain than seems normal for an ear infection. For instance, if your child won't stop crying, that may be a reason to talk to the child's doctor.
-
4Go if you notice drainage. Drainage in both adults and children is a sign that you need to go to the doctor. Drainage is a symptom of a ruptured eardrum, and your doctor will need to check out your ear to see if you need treatment, such as antibiotics.[17]
- If you are having drainage, you should avoid swimming until the infection is cleared up.
-
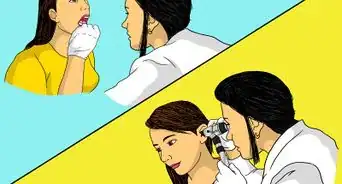
5Expect your doctor to perform certain tests. Your doctor will likely start by examining you or your child's eardrum with an otoscope, which just means the doctor will visually inspect the eardrum using an instrument. While doing so, the doctor may also blow a puff of air on the eardrum, to see if it moves like it should.[18]
- Your doctor might also use tympanometry. This test checks to see if there's fluid in the eardrum with pressure and air.
- With persistent ear infections, you or your child might have a hearing test to see if there's hearing loss.
-
6Understand your doctor may not do anything. That is, many ear infections go away on their own, and many doctors are trying to prescribe fewer antibiotics due to bacteria's adaptive nature. In addition, some ear infections are caused by viruses. Either way, antibiotics are not always needed, as ear infections generally clear up in a few days.[19]
- In addition, ear infections are not contagious, though viruses that can accompany ear infections sometimes are.
- Even after ear infections clear up, fluid can stay in the middle ear. It can remain there for a couple of months.
- However, you can help with the pain by using ibuprofen or acetaminophen. Be sure to use children's versions of these drugs for your child.
-
7Visit the hospital if you or your child experience facial paralysis. One rare complication of ear infections is a facial paralysis, when the swelling from the condition presses on the facial nerve. While this condition usually resolves when the ear infection clears up, it's still imperative to get any facial paralysis checked out by a doctor.[20]
-
8Go to the hospital if you or your child develop pain behind the ear. One complication that can arise from an ear infection is the spreading of the infection to other parts of the body. When you or your child develops pain behind the ear, that could be an indication that the infection has spread to the bone under the ear, the mastoids, an infection called mastoiditis. You may also notice hearing loss, pain, and discharge.[21]
- This condition is generally treated in the hospital.
-
9Go to the emergency room if you or child develops signs of meningitis. Rarely, an ear infection can develop into meningitis. You may notice you have a high fever, trouble breathing, and a bad headache. You may also have a stiff neck or feel nauseated. You may develop sensitivity to light, as well as a red, splotchy rash. If you notice these symptoms in you or your child, go to the emergency room or dial emergency services.[22]
-
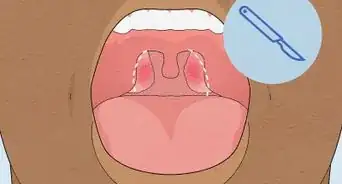
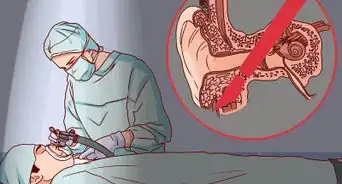
10Consider ear tube surgery. If your child has persistent ear infections, your doctor may consider ear tube surgery. Usually, this procedure is performed if your child has hearing loss or speech delays due to hearing loss. Basically, a tube is inserted in the ear so that fluid can drain more readily.[23]
- The presence of the tiny hole in the eardrum will not affect hearing. Tubes will remain in place six to 18 months, depending on the type used.[24]
Knowing the Risk Factors
-
1Understand age is a risk factor. Because children are not fully grown, their ear tubes are smaller and have a more horizontal angle than adults' ears. This shape and structure makes it more likely that their ears will develop an obstruction of some kind and get infected. Children ages 6 months to two years of age are most prone to ear infections.[25]
-
2Know that colds can lead to ear infections. The virus causing your cold can travel through the Eustachian tube that connects your ear to the back of your nose. If this happens to you or your child, you or your child can develop an ear infection while also having a cold.[26]
- Group daycares are a hot spot for ear infections. When your kids run around with other kids, some of whom may have colds, they are more likely to a catch a cold themselves.
- Be sure to get the recommended vaccinations, such as the flu vaccine once year, as that can protect against infections that could lead to ear infections.
-
3Understand the season can play a role. Generally, children catch ear infections more often in the fall and winter. This phenomenon is due to the fact that cold and flu infections are more prevalent this time of year, which, as noted, can lead to ear infections.[27]
- Similarly, if you or your child is prone to allergies, you are more likely to develop an ear infection when allergy counts are higher.
-
4Look for snoring or mouth-breathing. These symptoms can indicate that your child (or you) has large adenoids. Having this condition can put you or your child at risk for more ear infections. Talk to your doctor if you notice this symptom, as you or your child may need surgery to fix it.[28]
Preventing Ear Infections
-
1Breastfeed your baby for a year. Breastfed children are less likely to develop ear infections. Try to breastfeed for the first six months at least, but breastfeeding for a full year is better if you are able to manage it. Your breast milk provides your child with antibodies that help fight off ear infections.[29]
-
2Feed your child sitting up. When children lay down to drink a bottle, they are more likely to develop an ear infection. When the child is on their back, fluid can flow into their ears, which can cause an infection. Make sure your child is at a 45-degree angle when drinking from a bottle.[30]
-
3Work on allergies. Those prone to allergies are more likely to develop ear infections, both children and adults. If you can work on controlling allergies, you can help reduce the likelihood that you or your child will develop an ear infection.[31]
- You can take antihistamines to help reduce your allergies, as well as trying to avoid spending long periods outdoors when allergy counts are high.
- Stay hydrated to thin mucus and consider using a steam treatment or humidifier to help loosen mucus.[32]
- If your allergies are severe, talk to your doctor about other treatments.
-
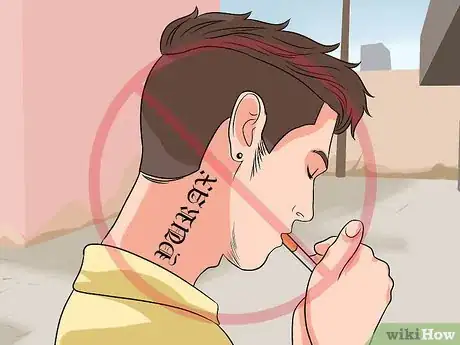
4Skip the cigarette smoke. You and your child should avoid cigarette smoke for many health-related reasons, but one in particular is that exposure to cigarette smoke can increase your chances of developing ear infections. Try to avoid all cigarette smoke, including secondhand smoke.[33]
- Bad air quality can have similar effects as cigarette smoke, increasing the risk for ear infections.[34]
References
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/otitis-media
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ https://www.nationwidechildrens.org/conditions/ear-infections-otitis-media
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ https://www.nationwidechildrens.org/conditions/ear-infections-otitis-media
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/otitis-media
- ↑ http://kidshealth.org/en/parents/otitis-media.html#
- ↑ http://kidshealth.org/en/parents/otitis-media.html#
- ↑ http://kidshealth.org/en/parents/otitis-media.html#
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ https://urgentcaresouthaven.com/when-should-you-go-to-the-doctor-for-an-ear-infection/
- ↑ http://www.cdc.gov/getsmart/community/for-patients/common-illnesses/ear-infection.html
- ↑ http://www.mayoclinic.org/diseases-conditions/ear-infections/symptoms-causes/dxc-20199484
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ http://kidshealth.org/en/parents/otitis-media.html#
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4553351/
- ↑ http://www.nhs.uk/Conditions/Otitis-media/Pages/Complications.aspx
- ↑ https://www.stanfordchildrens.org/en/topic/default?id=meningitis-in-children-90-P02528
- ↑ http://kidshealth.org/en/parents/otitis-media.html#
- ↑ http://kidshealth.org/en/parents/ear-infections.html#
- ↑ http://www.mayoclinic.org/diseases-conditions/ear-infections/symptoms-causes/dxc-20199484
- ↑ http://www.cdc.gov/getsmart/antibiotic-use/uri/ear-infection.html.
- ↑ http://www.mayoclinic.org/diseases-conditions/ear-infections/symptoms-causes/dxc-20199484
- ↑ http://my.clevelandclinic.org/childrens-hospital/health-info/diseases-conditions/hic-Otitis-Media
- ↑ https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media/prevention
- ↑ https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media/prevention
- ↑ https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media/prevention
- ↑ http://www.aafp.org/afp/2007/1201/p1659.html
- ↑ https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media/prevention
- ↑ http://www.mayoclinic.org/diseases-conditions/ear-infections/symptoms-causes/dxc-20199484

















































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...