X
This article was medically reviewed by Janice Litza, MD and by wikiHow staff writer, Megaera Lorenz, PhD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 34,213 times.
Fistulas can be painful, but fortunately, they can often be treated by a doctor. Our guide will help you recognize the symptoms as well as prepare for the exams, tests, and treatment options your doctor might offer.
Steps
Part 1
Part 1 of 3:
Recognizing Fistula Symptoms
-
1Check for pain around the anus or genitals. Pain and irritation are common symptoms of many types of fistulas. You may experience pain and swelling around anus, genitals, or the area between the genitals and anus (the perineum).[1]
-
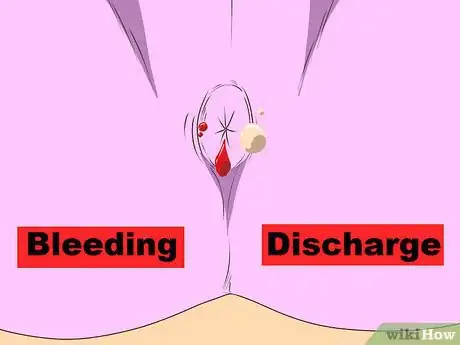
2Look for unusual bleeding or discharge. Fistulas may cause bleeding or discharge around the anus or genitals. You may notice that the discharge is foul-smelling, or that it contains pus.[4]
- If you have a vaginal fistula, you may have vaginal discharge that contains pus or feces. You might also notice gas leakage from your vagina.
Advertisement -
3Make note of urinary problems. Fistulas involving the bladder can cause a variety of urinary tract symptoms. In addition to frequent urinary tract infections, you may experience:
- Difficulty holding your urine, or leakage of urine from unusual places (e.g., your vagina).
- The passage of gas from your urethra (the opening between your bladder and your genitals) when you pee.
- Discolored, cloudy, or bad-smelling urine.
-
4Watch for gastrointestinal symptoms. Fistulas can cause pain in the pelvis or abdomen. You might also notice nausea, diarrhea, or vomiting. While these can be symptoms of many different conditions, they may indicate a fistula if you experience them in combination with other common fistula symptoms (such as genital pain and discharge).[5]
-
5Note any general symptoms of illness. In addition to more specific symptoms, fistulas can cause vague symptoms that affect your whole body. These symptoms may indicate an infection associated with the fistula. You might notice symptoms such as:[6]
- Fever.
- Chills.
- Fatigue.
- A general feeling of being ill.
Advertisement
Part 2
Part 2 of 3:
Getting a Medical Diagnosis
-
1Make an appointment to see your primary care physician. If you think you may have a fistula, call your doctor right away. If left untreated, a fistula can lead to infection or further damage to the surrounding tissues.[7] At your appointment, tell your doctor about:
- Any symptoms you are currently experiencing.
- Your overall health history and any other medical conditions you may have.
- Any medications you are currently taking.
-
2Let your doctor perform a physical. Your doctor will start by doing a physical exam to check for any visible signs of a fistula. They may also feel for any obvious masses, areas of tenderness, or other signs of illness, infection, or injury.
- For suspected vaginal fistulas, your doctor may perform a pelvic exam and use a speculum to look inside your vagina.[8]
- For fistulas involving the anus or rectum, the doctor may need to feel the inside of your rectum digitally (with their gloved fingers) or look inside your anus and rectum with an instrument called an anoscope.[9]
- Anal fistulas may be visible externally as openings in the skin around your anus.[10]
-
3Consent to imaging tests. If your doctor suspects a fistula, they will probably recommend 1 or more imaging tests to determine the location of the fistula. Common imaging tests include:[11]
- X-rays of the rectum, urinary tract, and genitals. You will need to take an injection or enema made of a contrast material (such as barium or radioactive iodine) in order to make any possible fistulas visible on the X-rays.
- CT-scans or MRIs.
- An ultrasound of the anus or vagina.
-
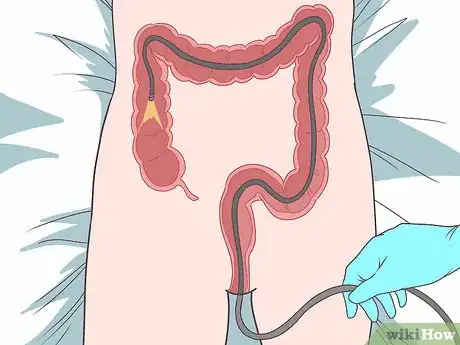
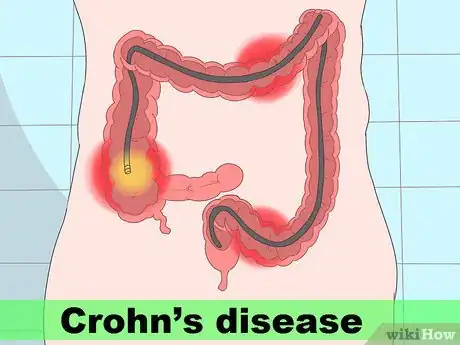
4Get a colonoscopy, if your doctor recommends it. If your doctor suspects you may have fistulas caused by Crohn's disease or another inflammatory bowel disorder, they may want to perform a colonoscopy. This involves inserting a tiny camera into the colon through the anus using a long, flexible tube.[12]
- Most commonly, colonoscopies are performed under “conscious sedation.” This means that you will be semi-conscious during the procedure, but should not feel any major discomfort.
-
5Provide blood samples, if needed. For some types of fistulas, it may be useful to do blood tests. Blood tests can be useful for identifying Crohn's disease (a common cause of fistulas).[13]
-
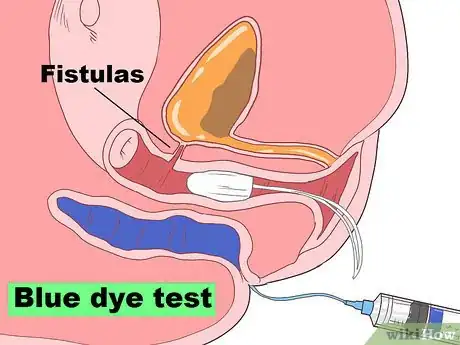
6Get a double-dye or blue dye test for vaginal fistulas. These tests are used to diagnose fistulas involving the vagina and bladder or rectum. You may be asked to swallow a brightly colored dye, and/or have the dye injected into your rectum or bladder. Then, you will insert a tampon into your vagina. If the tampon picks up any of the dye, that will provide a clue to the location of the fistula.
-
7
-
8Discuss your treatment options. The right treatment for your fistula will depend on the fistula's size, location, and any other related complications. Your doctor may refer you to another specialist, such as a urologist or gynecologist, for treatment. Common treatments include:[18]
- A small catheter inserted into the fistula to drain any infected material, blockages, or built up fluid.
- Antibiotics to treat infection.
- Surgery to repair the fistula.
- The use of special medicinal glues or other materials (such as collagen) to seal or fill the fistula.
- For fistulas between the anus and the surface of the skin, it may be possible to encourage the fistula to heal by making a small incision in the skin and muscle over the fistula.[19]
Advertisement
Part 3
Part 3 of 3:
Assessing Your Risk Factors
-
1Determine if you have an inflammatory bowel condition. Inflammatory bowel diseases, such as Crohn's disease or ulcerative colitis, can increase your risk of developing some types of fistulas.[20] If you have symptoms of a fistula and you also know or suspect that you have an inflammatory bowel condition, let your doctor know.
- You may have IBD if you experience persistent diarrhea, abdominal cramps, bloating, bloody stools, fever, nausea, and unexplained weight loss.
- Diverticulitis, a condition in which small pockets form in the colon and become inflamed or infected, can also lead to fistulas.[21]
-
2Look at your childbirth history, if applicable. Fistulas can occur during a difficult or complicated childbirth. Fistulas between the rectum and vagina are particularly common, but you might also develop fistulas around the outside of the anus.[22] After childbirth, follow up regularly with your OB-GYN to make sure any injuries associated with the delivery process are healing up properly.
- Call your OB-GYN right away if you have recently given birth and are experiencing any symptoms of an infection or fistula, such as fever, pain, or bad-smelling discharge.
-
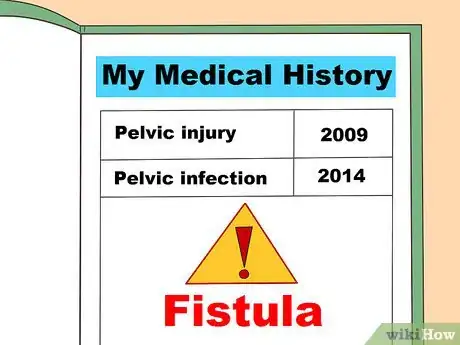
3Examine any history of pelvic injury or infection. Any kind of injury to your bowels or pelvic region can put you at risk of developing a fistula. This type of injury may result from trauma (for example, an injury caused by a car accident) or from a complicated pelvic surgery (such as a hysterectomy). You can also develop fistulas as a result of infection, cancer, or radiation therapy that affects your pelvis.[23]
- Injuries due to radiation therapy may take a long time to develop. If you've had pelvic radiation treatment, you may develop a fistula 6 months to 2 years later.
- Some types of sexually transmitted infections, such as chlamydia and HIV, may put you at greater risk of developing a fistula.[24]
Advertisement
References
- ↑ https://www.nhs.uk/conditions/anal-fistula/
- ↑ https://my.clevelandclinic.org/health/diseases/14466-anal-fistula
- ↑ https://www.mountsinai.org/care/obgyn/services/fistula-care
- ↑ https://www.nhs.uk/conditions/anal-fistula/
- ↑ https://www.uclahealth.org/medical-services/womens-pelvic-health/conditions-treated/fistulas
- ↑ https://my.clevelandclinic.org/health/diseases/14466-anal-fistula
- ↑ https://www.uclahealth.org/medical-services/womens-pelvic-health/conditions-treated/fistulas
- ↑ https://www.mayoclinic.org/diseases-conditions/rectovaginal-fistula/diagnosis-treatment/drc-20377113
- ↑ https://my.clevelandclinic.org/health/diseases/14466-anal-fistula/diagnosis-and-tests
- ↑ https://my.clevelandclinic.org/health/diseases/14466-anal-fistula/diagnosis-and-tests
- ↑ https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=tn10138
- ↑ https://my.clevelandclinic.org/health/diseases/14466-anal-fistula/diagnosis-and-tests
- ↑ https://my.clevelandclinic.org/health/diseases/14466-anal-fistula/diagnosis-and-tests
- ↑ https://emedicine.medscape.com/article/452934-workup#c6
- ↑ https://www.mayoclinic.org/diseases-conditions/rectovaginal-fistula/diagnosis-treatment/drc-20377113
- ↑ https://www.nhs.uk/conditions/anal-fistula/
- ↑ https://www.mayoclinic.org/diseases-conditions/rectovaginal-fistula/diagnosis-treatment/drc-20377113
- ↑ https://www.nhs.uk/conditions/anal-fistula/treatment/
- ↑ https://my.clevelandclinic.org/health/diseases/14466-anal-fistula/management-and-treatment
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2967329/
- ↑ https://colorectal.surgery.ucsf.edu/conditions--procedures/diverticulitis.aspx
- ↑ https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=tn10138
- ↑ https://www.uclahealth.org/medical-services/womens-pelvic-health/conditions-treated/fistulas
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4223259/
About This Article
Advertisement





























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...