This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 14 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 97,870 times.
The vagus nerve, also called the 10th cranial nerve and the X cranial, is the most complex of the cranial nerves. The vagus nerve is responsible for telling your stomach muscles to contract when you eat so you can digest your food. When it's not working, it can lead to a condition called gastroparesis, which is when your stomach empties more slowly than it should.[1] To tell if your vagus nerve is damaged, watch for symptoms of gastroparesis, and then talk to your doctor, who may order diagnostic tests for you.
Things You Should Know
- Nausea, vomiting, slow digestion, heartburn, low appetite, weight loss, and bloating are all symptoms of gastroparesis.
- Go to the doctor if you experience more than one symptom at once for more than a week. Gastroparesis can cause serious dehydration.
- Get an official diagnosis if necessary. Typically, this will involve an X-ray test or a gastric emptying study.
Steps
Gastroparesis Symptoms
-
1Notice if it’s taking longer for food to go through your system. Gastroparesis prevents food from moving through your body at a regular pace. If you notice you’re not going to the bathroom as frequently, it could be a sign that you have gastroparesis.[2]
-
2Pay attention to nausea and vomiting. Nausea and vomiting are common symptoms of gastroparesis. Because your stomach is not emptying as it should, the food is just sitting there, which makes you nauseous. In fact, when you vomit, you may notice the food hasn't been digested at all.[3]
- This symptom will likely be a daily occurrence.
Advertisement -
3Notice heartburn. Heartburn is also a common symptom of this disease. Heartburn is a burning sensation in the chest and throat, caused by acid coming back up from your stomach. You'll likely have this symptom regularly.[4]
-
4Check if your appetite is low. This disease can decrease your appetite, as the food you eat isn't being digested properly. That means that new food has nowhere to go, so you won't feel as hungry. In fact, you may feel full after a few bites when you do eat.[5]
-
5Watch for weight loss. Because you won't want to eat as much, you may lose weight. Plus, your stomach isn't digesting the food as it should, so you're not getting the nutrients you need to fuel your body and help you keep weight on.[6]
-
6Look for pain and bloating in your stomach. Because food sits in your stomach longer than it should, you may experience the feeling of being bloated. Similarly, this condition can also give you a stomachache.[7]
-
7Be aware in blood sugar changes if you're a diabetic. This disease is common in type 1 and type 2 diabetics. If you notice your blood sugar readings are more erratic than normal, that could also be a symptom of this issue.[8]
Speaking to Your Doctor
-
1Visit the doctor if you notice a combination of symptoms. Make an appointment to see your doctor if you notice these symptoms together for more than a week, as this disease can have serious complications. It can lead to you becoming dehydrated or malnourished, as your body isn't getting what it needs through digestion.[9]
-
2Make a list of your symptoms. Whenever you go to the doctor, it's a good idea to make a list of your symptoms. Write down the symptoms you've been having and when, so your doctor can get a good idea of what's going on with you. Plus, it will help you remember everything you need to when you get to the doctor's office.[10]
-
3Expect a physical examination and diagnostic tests. The doctor will ask you questions about your medical history, as well as give you a physical exam. They will likely feel your stomach and use a stethoscope to listen to the area. They may also do imaging studies to help figure out what’s causing your symptoms.[11]
- Bring up any risk factors, which include diabetes and abdominal surgery. Other risk factors include hypothyroidism, infections, nerve disorders, and scleroderma.
Getting Tested
-
1Be ready for an endoscopy or X-rays. The doctor will likely order these tests first to make sure you don't have a stomach blockage. A stomach blockage can cause symptoms that are similar to gastroparesis.[12]
- For an endoscopy, your doctor will use a tiny camera on a flexible tube. You'll first be given a sedative and likely a throat-numbing spray. The tube will be threaded down the back of your throat and into your esophagus and upper digestive tract. The camera will help your doctor see what's going on more directly than they can with an X-ray.[13]
- You may also receive a similar test called an esophageal manometry test to measure stomach contractions. In this case, the tube will be inserted through your nose and left in for 15 minutes.[14]
-
2Expect a gastric emptying study. If the doctor doesn't see a blockage in the other tests, they'll likely order this study. This test is a bit more interesting. You'll eat something (such as a an egg sandwich) that has a low dose of radiation. Then the doctor will look at how long it takes you to digest it by using an imaging machine.[15]
- Typically, you'll get a diagnosis of gastroparesis if half the food is still in your stomach after an hour to an hour and a half.
-
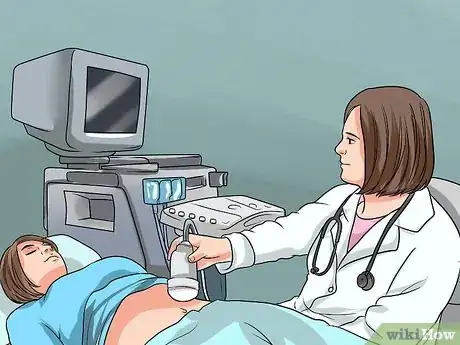
3Ask about an ultrasound. An ultrasound will help the doctor detect if some other issue is causing your symptoms. Particularly, they will look at how well your kidneys and gallbladder are functioning with this test.[16]
-
4Be ready for an electrogastrogram. If the doctor is having a hard time explaining your symptoms, you'll likely have this test done. Basically, it's a way of listening to your stomach for an hour. They'll put electrodes on the outside of your belly. You must have an empty stomach for this test.[17]
References
- ↑ https://www.nhs.uk/conditions/gastroparesis/
- ↑ https://my.clevelandclinic.org/health/diseases/15522-gastroparesis
- ↑ https://my.clevelandclinic.org/health/diseases/15522-gastroparesis
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/gastroparesis/symptoms-causes
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/gastroparesis/symptoms-causes
- ↑ https://medlineplus.gov/ency/article/000297.htm
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/gastroparesis/symptoms-causes
- ↑ https://my.clevelandclinic.org/health/articles/gastroparesis-overview
- ↑ https://www.nhs.uk/conditions/gastroparesis/
- ↑ https://www.nhs.uk/conditions/gastroparesis/
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/gastroparesis/diagnosis
- ↑ https://my.clevelandclinic.org/health/articles/gastroparesis-overview
- ↑ https://www.ucsfhealth.org/conditions/gastroparesis/diagnosis.html
- ↑ https://my.clevelandclinic.org/health/articles/esophageal-manometry-test
- ↑ https://www.ucsfhealth.org/conditions/gastroparesis/diagnosis.html
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/gastroparesis/diagnosis
- ↑ https://www.ucsfhealth.org/conditions/gastroparesis/diagnosis.html







































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...