This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 12 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 84% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 1,440,007 times.
Vaginal discharge is a common symptom in women and is most often completely normal and a sign that the vagina is functioning properly. Your vagina has a naturally acidic pH in order to protect you against infection. A healthy vagina regularly secretes discharge that in turn carries away dead cells and bacteria from your body. However, it's important to note that vaginal discharge can, in certain cases, be a symptom of infection or disease. Being able to discern normal from abnormal vaginal discharge is key to maintaining good vaginal health.
Steps
Self-Diagnosing Normal Vaginal Discharge
-
1Understand the function of vaginal discharge. The vagina has a specialized lining, which contains glands that excrete small amounts of fluid every day. The purpose of regular, daily vaginal discharge is to collect old, sloughed cells and possible pathogens or "foreign bodies", and to expel them from the vagina. In addition, this discharge encourages a healthy balance of bacteria and yeast which protects against infection.
- In other words, most vaginal discharge is good for you. Discharge is a natural way that your body protects itself.
- Women will have a normal discharge every 80 minutes during sleep. This is a normal physiologic function (men as well have an erection every 80 minutes during sleep).
-
2Understand what normal vaginal discharge looks like. Normal vaginal discharge is usually clear or milky-white and may have a mild, if any, odor. It can be watery or thick and mucus-y, but the consistency should be relatively smooth and lump free most of the time.[1]
- In premenopausal women, it is normal to have about 1 teaspoon of white or clear vaginal discharge every day.[2] However, the amount and characteristics of vaginal discharge can vary from one woman to another.
Advertisement -
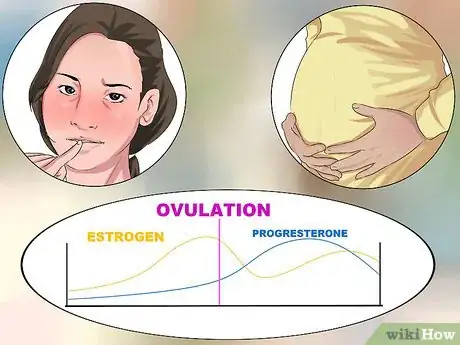
3Know the normal reasons your discharge may change. There are a number of reasons that your vaginal discharge may look, smell or appear slightly different. If you're concerned about your discharge, run through this quick check list to see if you are experiencing or have recently experienced any of the following conditions. These are the most common - but completely normal - reasons your discharge may change:
- Ovulation: During ovulation, there is usually an increased volume of discharge. This discharge is more clear, stretchy, and slippery. The purpose of this change is to allow easier passage of sperm during the time that an egg is ready for fertilization.[3]
- Menstruation: Discharge that is thick and white typically makes an appearance just before and after your menstrual cycle.[4]
- Pregnancy and post-partum: Pregnant women often notice an increase in the amount of discharge and a change in its consistency. This is especially noticeable in the last few weeks before delivery, when discharge can become thicker and more voluminous. After delivery, women will experience discharge termed “lochia." This particular discharge consists of blood, small clots, and sloughed-off tissue from the lining of the uterus that built-up over the course of pregnancy. Over time, it will change into a watery, pink discharge and eventually subside.[5]
- Menopause: The normal amount of vaginal discharge typically decreases during menopause as estrogen levels fall.[6]
- Sexual arousal: Watery discharge that is clear or slightly white is a sign of sexual excitement. The purpose of this discharge is to provide lubrication to protect the vagina during sex.[7]
-
4Don't worry about "cleaning out" your normal discharge. Your discharge is your body’s natural way of protecting itself. Douching is advisable only on rare occasions.
- If you don't like the feeling of wetness on your underwear and clothing, consider wearing a panty-liner in your underwear. These can be purchased at grocery stores, drug stores and pharmacies, and convenience stores. You can also make your own pantyliners out of fabrics you have around the house, or bought from a craft store, if you want a cheaper and more natural solution.
Self-Diagnosing Abnormal Vaginal Discharge
-
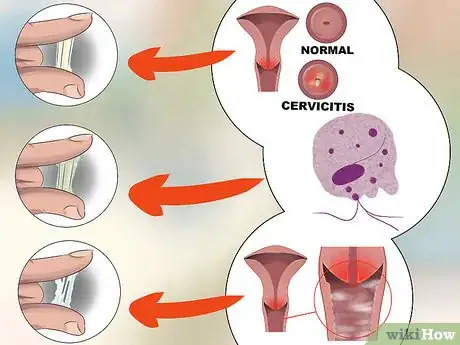
1Examine the color and texture of your vaginal discharge. If it looks different from the vaginal discharge you usually secrete, then there is a chance that it is abnormal and a symptom of an infection or change in the vaginal environment. A good rule of thumb is that if the discharge isn't clear or white, then you may have a problem. The most common symptoms of a pathology include: [8]
- White, thick, lumpy discharge that is itchy.
- Green and foamy discharge.
- Grayish, yellowish, brownish or greenish discharge.
- Foul-smelling discharge.
- Discharge accompanied by pain, itchiness or burning, bleeding, etc.
- Discharge that it is heavier or thicker than usual.
-
2Evaluate the vaginal discharge. Having examined the discharge, now assess which of the conditions that can cause abnormal discharge may apply to you. If your discharge does not fall in the ‘normal’ range of colors and textures, it may be a result of one of the following:
- Bacterial vaginosis: This is the most common cause of abnormal discharge in women of childbearing age. Bacterial vaginosis is a mild vaginal infection caused by "bad" bacteria. Essentially there are "good" and bad types of bacteria and the good types help to regulate the growth of the bad types. In cases of bacterial vaginosis this balance is upset and there are too many bad bacteria. Symptoms include grayish-yellow, slippery, and fishy-smelling discharge as well as itching or burning in the vagina. Most discharges with odor are due to bacterial vaginosis.[9]
- Vaginal candidiasis (yeast infection): If your discharge is white but thick and lumpy (think cottage cheese), it could be a sign of a yeast infection. In addition to the change in texture and color, you may also notice itching and burning sensations. Yeast infections do not usually produce a strong scent. These infections are the second most common type of vaginal infection among women. They are particularly likely to occur after a regimen of antibiotics, in patients with diabetes or immunocompromised patients.[10]
- Trichomoniasis: Discharge that is slightly green in hue and ‘frothy’ in texture is typically a symptom of trichomoniasis. Trichomoniasis is an infection with trichomonas, a single-cell parasite which is passed between sexual partners. This infection, the third most common infection that can affect your vaginal discharge, can also cause vaginal itching or pain.[11]
- STIs (Sexually Transmitted Infections): The common STIs chlamydia and gonorrhea can sometimes have the sole symptom of increased vaginal discharge. The characteristics of this discharge can vary, but it is often discolored (i.e. gray, yellow, green), thick, and foul-smelling. Women may also notice pain during sexual activity, as well as spotting or brown discharge afterward.[12] Bacterial vaginosis, Candidiasis, and Trichomoniasis can also be spread sexually.
- Vaginal or cervical cancer: Keep in mind that cancer of the vagina or cervix is a very rare cause of abnormal discharge.[13]
-
3Consider other causes of abnormal discharge. There are a lot of things than can affect the vaginal environment.
- Exposing the vagina to a new type of cleaning agent or hygiene product can have an effect on it. Chemicals found in detergents and fabric softeners, feminine sprays, creams, douches, and contraceptive foams or jellies or creams may irritate the vagina and/or the skin around the vagina. Medications, such as antibiotics, can also increase the possibility of infection. Any of these may be causing your symptoms and the changes in your vaginal discharge. Think about what you have used most recently and when your discharge began to seem different to you. Once you are able to narrow the potential cause down, try eliminating it and seeing if your symptoms disappear. For example, if you recently changed to a new laundry detergent, avoid using it for a while and return to your old brand. If your symptoms go away, then you may have found the culprit! If your symptoms persist, however, even after you've considered any new chemicals that may have recently been added to your environment, you should visit your doctor. [14]
- Systemic illnesses that can also alter the balance of the vaginal environment. For example, women with diabetes have an increased risk of fungal infections (like yeast infections).[15]
- A not uncommon cause of vaginal discharge with a foul odor is a tampon that has been left in and forgotten. If you suspect that you may have left a tampon inside of yourself, you can do your own investigation. Begin by washing your hands and then squatting or placing one foot on the edge of your bathtub or toilet. Reach up inside your vagina as far as you can reach and feel around for anything. If you find a tampon but can't locate the string to pull it out, then use your finger and thumb to grab onto it and pull it out. Make sure the tampon is still generally intact; if it has started to disintegrate and you are unsure that you pulled all of the pieces out, contact your doctor as nothing should be left behind. Note that if you feel all the way up to your cervix and find nothing, there is likely nothing up there. If you still suspect that there is something up there but that you couldn't find it, contact your doctor, who can do a more thorough check for you.[16]
-
4Consult your physician. If after self-examination, you believe your discharge is abnormal, visit your doctor. Though it's useful to pay attention to your body and its many changes, don't rely on your own diagnosis as confirmation of particular condition. Let your health care provider examine you, run any necessary tests, and decide on a course of action or treatment.[17]
- One exception here may be if you've had a yeast infection (Vaginal candidiasis) in the past and feel confident in your ability to self-diagnose this infection based on your previous experience. Treatments for yeast infection are readily available over-the-counter at pharmacies and drug stores and can be administered at home. However, if the infection persists after this over-the-counter, standard treatment for candidiasis, it is highly advisable that you visit your physician.
Getting Examined and Tested
-
1Make an appointment with your physician. You should try to see your doctor as soon as you notice or suspect that your vaginal discharge is abnormal. Be prepared to describe the color, consistency, and frequency of the discharge.
- If you are currently menstruating, it's best to wait until after your cycle finishes to see your doctor, if at all possible. But if there are significant symptoms, then be seen as soon as possible, even if menstruating.
- If you are visiting a walk-in clinic and not your regular doctor, be prepared to give a full medical history.
-
2Let the doctor know of any conditions or actions that may be relevant. For example, if you think you may be pregnant or recently had unprotected sex (i.e., sex without a condom), you should let your doctor know.
-
3Have a physical examination, including a pelvic exam.[18] Depending on your symptoms, your doctor may elect to do a partial pelvic exam or a full exam. A full exam includes an external and internal examination of the female pelvic organs:
- The External Exam — Your health care provider will examine the opening of your vagina and the folds of your vulva. In particular, your doctor is looking for abnormal discharge, cysts, genital warts, irritation, or other conditions.
- The Internal Exam (a) — The internal exam has two parts: the speculum exam and the bimanual exam. During the speculum exam, your doctor will gently insert a lubricated metal or plastic speculum into your vagina. The speculum separates the walls of the vagina when it opens. This should not feel painful but may feel slightly uncomfortable. Let your health care provider know if you do feel any pain. She may be able to adjust the size or position of the speculum. If there is a significant vaginal infection, the Pap test usually done at this time might be deferred, since the results of the Pap smear might be compromised. If so, you should return for a Pap test once the infection is cleared. In the Pap test, a tiny spatula or small brush to take a small sample of cells from your cervix. This sample will be examined to see if there are any cancerous or precancerous cells in the cervix. A sample of discharge from the cervix also may be taken from the vagina to test for STIs. In addition, your doctor will measure your vaginal pH and take samples of vaginal discharge for testing.[19]
- The Internal Exam (b) — The second test, the bimanual exam, involves your doctor inserting one or two gloved and lubricated fingers into your vagina while gently pressing on your lower abdomen with the other hand. This is a way to check for the size, shape, and position of the uterus, ovaries and fallopian tubes, which could affect your fertility and health. For example, an enlarged uterus could mean that you are pregnant or have fibroids, while pain or tenderness in the adnexa areas (ovary/tube) experienced during the exam could indicate an infection, cyst or possible mass.[20]
- Sometimes as part of a pelvic exam, your doctor may perform a rectal exam. In this instance, your doctor will put a gloved finger into the rectum to check for any tumors or other abnormalities. [21]
-
4Have your samples sent to a lab for testing. After the exam, your doctor will send all cultures and samples to the laboratory for testing. The most important test for samples of vaginal discharge is microscopic examination, or a wet prep test. In a wet prep test, a technician will mix the sample of vaginal discharge with saline and take a drop of this mixture and put it on a slide to examine. This is usually done in the doctor’s office, so results are available immediately.[22]
- The technician will carefully examine the slide at both medium and high power for trichomonas, clue cells, and yeast. Trichomonas are fluid, flagellated organisms that can be identified by their characteristic twisting motion. Clue cells are unusual cells whose existence in the sample means that bacterial vaginosis may be present. Lastly, yeast may be identified on the slide as budding or branching forms and is indicative of a yeast infection. The presence of yeast can also be determined through the Pap test.
-
5Wait for your test results. Make sure to find out when you should expect results from these tests so you can meet again with your doctor to development a treatment plan if needed.[23]
References
- ↑ http://kidshealth.org/teen/sexual_health/girls/vdischarge2.html
- ↑ https://www.sutterhealth.org/pamf/health/teens/female/vaginal-discharge
- ↑ https://patient.info/doctor/vaginal-discharge#ref-3
- ↑ https://www.sutterhealth.org/pamf/health/teens/female/vaginal-discharge
- ↑ https://medlineplus.gov/ency/article/003158.htm
- ↑ http://www.patient.info/doctor/vaginal-discharge
- ↑ https://medlineplus.gov/ency/article/003158.htm
- ↑ https://patient.info/doctor/vaginal-discharge#ref-3
- ↑ http://familydoctor.org/familydoctor/en/diseases-conditions/vaginal-discharge.printerview.all.html
- ↑ http://familydoctor.org/familydoctor/en/diseases-conditions/vaginal-discharge.printerview.all.html
- ↑ http://familydoctor.org/familydoctor/en/diseases-conditions/vaginal-discharge.printerview.all.html
- ↑ http://familydoctor.org/familydoctor/en/diseases-conditions/vaginal-discharge.printerview.all.html
- ↑ https://medlineplus.gov/ency/article/003158.htm
- ↑ https://medlineplus.gov/ency/article/003158.htm
- ↑ http://www.healthywomen.org/condition/yeast-infections
- ↑ https://www.healthdirect.gov.au/retained-object-or-tampon
- ↑ https://medlineplus.gov/ency/article/003158.htm
- ↑ https://www.msdmanuals.com/en-sg/home/quick-facts-women-s-health-issues/symptoms-of-gynecologic-disorders/vaginal-discharge
- ↑ http://www.plannedparenthood.org/learn/womens-health/pelvic-exam#sthash.X9uovE8E.dpuf
- ↑ http://www.plannedparenthood.org/learn/womens-health/pelvic-exam#sthash.X9uovE8E.dpuf
- ↑ http://www.plannedparenthood.org/learn/womens-health/pelvic-exam
- ↑ http://www.ncbi.nlm.nih.gov/books/NBK288/
- ↑ http://www.plannedparenthood.org/learn/womens-health/pelvic-exam#sthash.X9uovE8E.dpuf
About This Article
If you want to self-diagnose your vaginal discharge, keep in mind that it may change based on where you are in your ovulation cycle. However, if you notice that your vaginal discharge looks different than normal, you may have an infection. For example, you may have bacterial vaginosis if your discharge is grayish-yellow and smells like fish. Alternatively, if you notice thick and lumpy discharge, it could be a sign of a yeast infection. In general, vaginal discharge that isn't clear or white could be a sign that something's wrong, so go to your doctor if you believe your discharge is abnormal. For more tips from our Medical co-author, including how to get tested for abnormal vaginal discharge, keep reading.





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...