This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 37,526 times.
Psoriasis is a common skin condition that is caused by the build up of extra skin cells on the surface of your skin. This skin condition is persistent and chronic. If you have psoriasis, your symptoms may alternate between getting better and getting worse.[1] You can determine if you have this skin condition by recognizing the symptoms of psoriasis and by getting a physical exam done by your doctor. If you are diagnosed with psoriasis, you should learn your treatment options so you can manage this skin condition.
Steps
Recognizing the Symptoms of Psoriasis
-
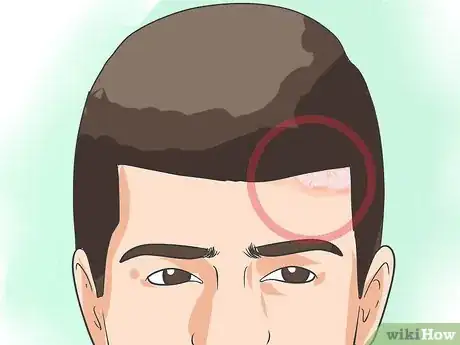
1Look for red patches of skin that appear scaly. You should look for any red patches of skin on your body, including your genitals and the inside of your mouth. The red patches may look like they are covered with silvery scales and may only appear in a few spots on your body or in large areas on your body. If you notice these symptoms, you may have a type of psoriasis called plaque psoriasis. This is the most common form of psoriasis.[2]
- You should also check along your hairline for red, itchy areas that have silvery-white scales. This is often a symptom of scalp psoriasis. You may also notice that you have flakes of dead skin in your hair or on your shoulder, especially after you have scratched at your scalp.
- Never treat plaque psoriasis with oral prednisone, because that leads to an increased risk of pustular psoriasis.
-
2Check if you have small, water-drop shaped sores on your body. This is a symptom of guttate psoriasis, which often affects young adults and children. The small, water-drop-shaped sores may appear on your arms, legs, scalp, and torso. The sores may be covered by a fine scale and may appear thin against your skin.[3]
- This type of psoriasis can be triggered by a bacterial infection like strep throat.
Advertisement -
3Look for smooth patches of inflamed skin. You should look for smooth patches of inflamed skin on your armpits, your groin, under your breasts, and around your genitals. This is a symptom of inverse psoriasis. This type of psoriasis often gets worse due to friction and sweating.[4]
- This type of psoriasis is often triggered by fungal infections. You can contract a fungal infection through contact with someone who has a fungal infection or through exposure to the infection in public showers, locker rooms, and pools.
-
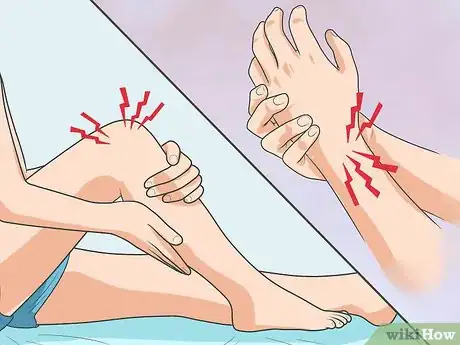
4Examine your hands, feet, and fingertips for blisters. The blister may appear to be filled with pus and the skin around the blisters may appear red and tender. These are symptoms of pustular psoriasis, a less common form of psoriasis.[5]
- If you have this type of psoriasis, you may also experience fever, chills, diarrhea, and severe itching.
-
5Check to see if your nails are thickened, pitted, or ridged. These are symptoms of nail psoriasis. If you have this type of psoriasis, you may also notice your nails are discolored and growing abnormally. Your nails may also become loose and separate from the nail bed, or it may crumble.[6]
-
6Note if your joints feel swollen or stiff. These could be symptoms of psoriatic arthritis. You may also have inflamed, scaly skin, and pitted, discolored nails. Your joints may feel very painful. Most people experience skin disease before joint disease, but for some people with psoriasis, their joints are affected first. Over time, this type of psoriasis can cause stiffness and joint damage.[7]
- Your symptoms may vary depending on if you have mild or severe psoriatic arthritis. But psoriatic arthritis can affect any joint.
-
7Ask yourself questions to determine your risk for psoriasis arthritis. The National Psoriasis Foundation developed this screening tool to determine if you’re at risk. If you answer yes to three of the following five questions you may have psoriasis arthritis:[8]
- Have you ever had a swollen joint?
- Has a doctor ever told you you have arthritis?
- Do your fingernails/toenails have holes or pits?
- Have you ever had pain in your heel?
- Have you ever had a finger or toe swollen or painful for no reason?
-
8Determine if your symptoms flare up every few weeks or months. Most types of psoriasis will flare up for a few weeks or months and then go into remission. You may notice your symptoms appearing in cycles, with a flare up and then a remission, where your symptoms subside for a time.[9]
- You may keep a journal of your symptoms to track how often your psoriasis flares up. You may also note when or if your psoriasis is in remission in your journal.
- If you feel your symptoms continue to flare up and then subside on a consistent basis, you likely have a form of psoriasis and should be examined by your doctor to confirm your diagnosis.
Getting Examined By Your Doctor
-
1Let your doctor do a physical exam of your skin. Your doctor can determine if you have psoriasis by looking at your skin, scalp, and nails. They may check for any red, scaly patches or inflamed areas on your skin. They may also look at your nails to check if they are pitted, discolored, or ridged.[10]
- Your doctor may ask you about your symptoms to help diagnose your issue. They may also consider your medical history to see if you are prone to skin conditions or have sensitive skin.
-
2Get a skin biopsy. Your doctor may take a small sample of your skin, called a biopsy to confirm the diagnosis. A biopsy can also help your doctor determine the type of psoriasis you have and rule out other disorders.[11]
- A skin biopsy is often done at the doctor’s office. An anesthetic may be applied to the area so you do not feel the removal of the skin sample. The results of the biopsy are often ready within a week.
-
3Allow your doctor to rule out other skin conditions. Your doctor should be able to use the results of the skin biopsy and the physical exam to make sure you have psoriasis and not other skin conditions. There are several skin conditions that look similar to psoriasis, including:
- Seborrheic dermatitis: This skin condition causes your skin to appear greasy, itchy, scaly, and red. You may notice seborrheic dermatitis on your face, upper chest, and back.[12]
- Lichen planus: This skin condition often appears as red, itchy bumps or lesions on your arms and legs.
- Ringworm: This skin condition is caused by a fungal infection. You may develop red, scaly rashes in a ring or circle.
- Pityriasis rosea: This skin condition appears as one large spot on your chest, abdomen, or back. It may then spread, forming the shape of drooping pine tree branches.[13]
Treating Psoriasis
-
1Talk to your doctor about topical treatments. There is no cure for psoriasis, so most treatments focus on removing the scaly layer of your skin so it is smooth and not irritated. The treatment may also prevent skin cells from growing too quickly, which can reduce inflammation and the formation of lesions. Your doctor may suggest topical treatments in the form of a cream or ointment as a first step to address your psoriasis, especially if it is mild.[14]
- Your doctor may suggest topical corticosteroids that you apply as a cream or ointment to your affected skin. Your doctor may also suggest a medicated cream that contains vitamin D analogues.
-
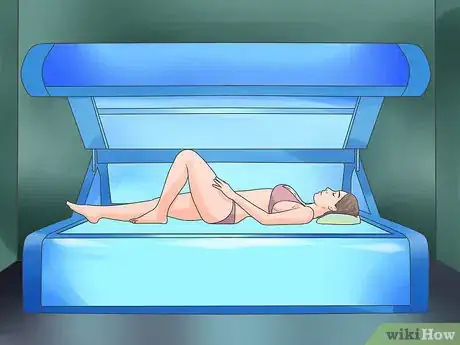
2Try light therapy. If your psoriasis is more severe or it does not go away with topical treatments, you doctor may suggest the use of light therapy or phototherapy. During light therapy, your skin is exposed to natural or artificial ultraviolet light in controlled doses.[15]
- Your doctor may refer you to a dermatologist, who will perform light therapy on your skin in their office. Depending on the severity of your psoriasis, you may need to do about 20 light therapy sessions before you see improvements on your skin.
- You can also try lying out in the sun as a form of light therapy. You may do multiple sunbathing sessions throughout the week to help treat your psoriasis. Make sure you wear SPF 15 and over on areas of your body that do not have psoriasis and avoid getting sunburnt, as sun burns can make psoriasis worse.[16]
-
3Get a prescription for oral medications. Your doctor may suggest oral medications or injected drugs if your psoriasis is very severe or resistant to other types of treatment. There are severe side effects for these medications so your doctor may only recommend that you use them for brief periods of time.[17]
- Your doctor may prescribe oral drugs like retinoids or methotrexate.[18] Your doctor may also suggest the use of injected drugs, which will help to treat psoriasis on your entire body. Other common drugs include ones that modify your immune system, such as adalimumab, etanercept, and infliximab.
Expert Q&A
-
QuestionWhat is the main cause of psoriasis?
 Lydia Shedlofsky, DODr. Lydia Shedlofsky is a Resident Dermatologist who joined Affiliated Dermatology in July of 2019 after completing a traditional rotating internship at Larkin Community Hospital in Miami, Florida. She earned a Bachelor of Science in Biology at Guilford College in Greensboro, North Carolina. After graduation, she moved to Beira, Mozambique, and worked as a research assistant and intern at a free clinic. She completed a Post-Baccalaureate program and subsequently earned a Master's Degree in Medical Education and a Doctorate of Osteopathic Medicine (DO) from the Lake Erie College of Osteopathic Medicine.
Lydia Shedlofsky, DODr. Lydia Shedlofsky is a Resident Dermatologist who joined Affiliated Dermatology in July of 2019 after completing a traditional rotating internship at Larkin Community Hospital in Miami, Florida. She earned a Bachelor of Science in Biology at Guilford College in Greensboro, North Carolina. After graduation, she moved to Beira, Mozambique, and worked as a research assistant and intern at a free clinic. She completed a Post-Baccalaureate program and subsequently earned a Master's Degree in Medical Education and a Doctorate of Osteopathic Medicine (DO) from the Lake Erie College of Osteopathic Medicine.
Dermatologist Psoriasis is really an autoimmune condition that happens to affect the skin, If you want to treat your skin, the best answer is to treat the condition itself. Beyond that, avoiding irritation to the skin with triggers such as scratching can help. Finally, I always recommend thick emollient lotions to be applied throughout the day, especially within the first few minutes after a shower.
Psoriasis is really an autoimmune condition that happens to affect the skin, If you want to treat your skin, the best answer is to treat the condition itself. Beyond that, avoiding irritation to the skin with triggers such as scratching can help. Finally, I always recommend thick emollient lotions to be applied throughout the day, especially within the first few minutes after a shower.
References
- ↑ https://www.psoriasis.org/about-psoriasis/
- ↑ https://my.clevelandclinic.org/health/diseases/6866-psoriasis#symptoms-and-causes
- ↑ https://www.aad.org/public/diseases/psoriasis/what/symptoms
- ↑ https://www.aad.org/public/diseases/psoriasis/what/symptoms
- ↑ https://www.aad.org/public/diseases/psoriasis/what/symptoms
- ↑ https://www.aad.org/public/diseases/psoriasis/what/symptoms
- ↑ https://www.aad.org/public/diseases/psoriasis/what/symptoms
- ↑ https://www.psoriasis.org/risk-for-psoriatic-arthritis/
- ↑ https://www.nhs.uk/conditions/psoriasis/symptoms/
- ↑ http://nyulangone.org/conditions/psoriasis/diagnosis
- ↑ http://nyulangone.org/conditions/psoriasis/diagnosis
- ↑ https://my.clevelandclinic.org/health/diseases/14403-seborrheic-dermatitis
- ↑ https://rarediseases.org/rare-diseases/pityriasis-rosea/
- ↑ https://www.nhs.uk/conditions/psoriasis/treatment/
- ↑ https://www.nhs.uk/conditions/psoriasis/treatment/
- ↑ https://www.psoriasis.org/phototherapy/
- ↑ https://www.nhs.uk/conditions/psoriasis/treatment/
- ↑ https://www.aad.org/public/diseases/psoriasis/treatment/medications































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...