This article was co-authored by Rebecca Levy-Gantt, MPT, DO. Dr. Rebecca Levy-Gantt is a board certified Obstetrician and Gynecologist running a private practice based in Napa, California. Dr. Levy-Gantt specializes in menopause, peri-menopause and hormonal management, including bio-Identical and compounded hormone treatments and alternative treatments. She is also a Nationally Certified Menopause Practitioner and is on the national listing of physicians who specialize in menopausal management. She received a Masters of Physical Therapy from Boston University and a Doctor of Osteopathic Medicine (DO) from the New York College of Osteopathic Medicine.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 12 testimonials and 90% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 989,266 times.
Miscarriage occurs when a pregnancy fails to progress before 20 weeks of gestation.[1] Miscarriages are common, impacting up to 25 percent of recognized pregnancies, and are nothing to be ashamed of.[2] To determine if you had a miscarriage, you'll need to evaluate your risk factors and monitor symptoms like heavy vaginal bleeding and pain. It can be difficult to determine if you had a miscarriage since some symptoms also occur in healthy pregnancies, however, so you should seek medical confirmation if you think miscarriage is a possibility. Always follow your physician's advice if you think you have suffered a miscarriage.
Steps
Miscarriage Causes and Symptoms
-
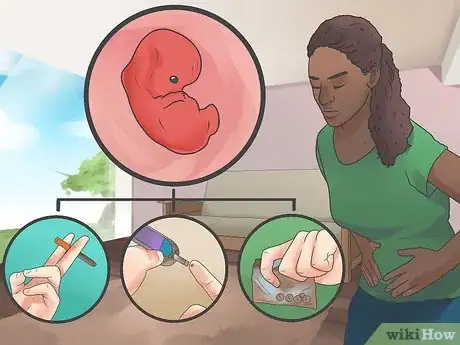
1Understand why miscarriages happen. Miscarriages most often occur in the early weeks of pregnancy. Chromosome abnormalities are the most common cause, and in most cases there's nothing the mother could have done to prevent it.[3] The risk of miscarriage drops after thirteen weeks of gestation. By then, most chromosome abnormalities would have already caused the pregnancy to end. The following factors also put people at higher risk of having a miscarriage: [4]
- Older women have a higher risk. Women who are 35 to 45 years old have a 20-30 percent chance of miscarriage, and women over the age of 45 have up to a 50 percent chance.
- Women with severe chronic illnesses, such as diabetes or lupus, have a higher risk of miscarrying.
- Abnormalities in the uterus, such as scar tissue, can lead to a miscarriage.
- Smoking, drug use and alcohol use can cause miscarriage to occur.
- Women who are overweight or underweight are at higher risk.
- Women who have already had more than one miscarriage are at higher risk.
-
2Check vaginal bleeding. Heavy vaginal bleeding is the most common sign that a miscarriage is occurring. It is often accompanied by cramps similar to those you might feel during your period.[5] The blood is typically brown or bright red in color.[6]
- Light spotting, and even moderate bleeding, can occur in healthy pregnancies. Heavy bleeding with clotting may indicate miscarriage. Notify your physician any time you experience bleeding during pregnancy.
- According to the some studies, 50 to 75 percent of miscarriages are chemical pregnancies. This means they occur shortly after implantation. Often, the woman does not realize she was pregnant and she experiences bleeding at the time her normal monthly period is due. Bleeding may be heavier than normal and cramping may be more severe.[7]
Advertisement -
3Check your vaginal mucous. Symptoms of miscarriage include pink-white vaginal mucous, which may contain pregnancy tissue. If your discharge looks like clotted tissue, or is solid in any way, this may be a sign that miscarriage is occurring or has occurred; you should see your doctor right away.
- Most pregnant women experience increased levels of clear or milky vaginal discharge called Leukorrhea.[8] If you have high levels of this type of discharge, there's no need for alarm.
- You may also mistake spot of urine for vaginal discharge. Urinary incontinence is a common occurrence in healthy pregnancies.
-
4Pay attention to your aches and pains. Any pregnancy brings a variety of aches and pains along with it. During a miscarriage, pain is usually located in the lower back and can range from mild to severe. If you experience lower back pain, talk with your physician right away.[9]
- Occasional twinges or aches in your abdomen, pelvic area and back are often the result of your body adjusting to accommodate your growing fetus. If pain is severe, persistent or occurs in waves you may be miscarrying, especially if there is also bleeding.
- It is also possible to experience "true contractions" if you're having a miscarriage. The contractions occur every 15 to 20 minutes, and are often severely painful.[10]
-
5Analyze your pregnancy symptoms. With pregnancy comes a slew of different symptoms, all caused by increased levels of hormones in your system. If you experience a reduction in symptoms, this may be a sign that a miscarriage has occurred and your hormone levels are returning to their pre-pregnancy state.
- If you've had a miscarriage you may notice less morning sickness, less swelling and tenderness of the breasts, and a feeling of no longer being pregnant. In healthy pregnancies, these early symptoms often subside on their own at about 13 weeks, which is also the time miscarriage risk decreases.
- Symptom occurrence and severity varies in every pregnancy. A sudden change prior to 13 weeks warrants a call to your physician's office.
-
6See your doctor to be sure. Visit your physician's office, emergency room, or the labor and delivery area of your hospital for a definitive answer as to whether you miscarried. Even if you experience all the above symptoms, there still may be a chance that the fetus can survive, depending on the type of miscarriage.
- Depending on how far your pregnancy has progressed, the physician will use blood tests, pelvic exam or ultrasound to check the viability of the pregnancy.
- If you experience heavy bleeding early in your pregnancy, your physician may not have you come in to the office unless you wish to do so.
Miscarriage Treatments
-
1Know the different types of miscarriage. Miscarriage affects every woman's body a little differently. In some cases all pregnancy tissues leave the body quickly, while in other cases the process is longer and a bit more difficult. Here are the different types of miscarriage, and what affect they have on the body:
- Threatened miscarriage: The cervix remains closed. It is possible that the bleeding and other miscarriage symptoms will stop, and the pregnancy will proceed as normal.[11]
- Inevitable miscarriage: Heavy bleeding occurs, and the cervix begins to open. At this point there is no chance that the pregnancy will continue.
- Incomplete miscarriage: Some pregnancy tissue leaves the body, but some stays inside. Sometimes a procedure is necessary to remove the remaining tissue.
- Complete miscarriage: All pregnancy tissue leaves the body.
- Missed abortion: Even though the pregnancy has ended, the tissue stays in the body. Sometimes it comes out on its own, and sometimes treatment is needed to remove it.[12]
- Ectopic pregnancy: This is not technically a type of miscarriage, but it is another type of pregnancy loss. Instead of implanting in the uterus, the egg implants in the fallopian tube or ovary, where it will not be able to grow.
-
2Call your physician if the bleeding stops on its own. If you experience heavy bleeding that eventually subsides, and it's still early in your pregnancy, you may not have to go to the hospital.[13] Many women prefer not have an extra hospital visit and would rather rest at home. This is usually fine as long as the bleeding stops within ten days to two weeks.
- If you're experiencing cramps or other pain, your physician might tell you how to make yourself more comfortable during the miscarriage.
- If you want to confirm that a miscarriage occurred, you can schedule an ultrasound.[14]
-
3Seek treatment if the bleeding doesn't stop. If you experience heavy bleeding and other miscarriage symptoms, and you are not sure whether the miscarriage is complete or incomplete, your physician may proceed using one of the following strategies:
- Expectant management: You'll wait and see whether the remaining tissue eventually passes and the bleeding stops on its own.
- Medical management: Medication is given to cause the remaining tissue to expel from the body. This requires a short hospital stay, and the bleeding that follows can last up to three weeks.
- Surgical management: Dilation and curettage, known as a D&C, is performed to remove the remaining tissue. The bleeding usually stops more quickly than it does for those who use the medical management method.[15] Medication may be administered to slow the bleeding.
-
4Watch your symptoms. If your bleeding continues past the time when your physician said it would slow and stop, it's important to seek treatment immediately. If you experience any other symptoms, such as chills or fever, see your doctor or go to the hospital right away.
-
5Look into grief counseling. Losing a pregnancy at any stage can be emotionally traumatic. It is important to grieve your loss, and seeking counseling can help. Ask your physician for a referral for grief counseling, or book an appointment with a therapist in your area.
- There is no certain amount of time after which you should feel better; it's different for every woman. Give yourself as much time as you need to grieve.
- When are ready to try to get pregnant again, talk with your physician about making an appointment with someone who specializes in high-risk pregnancies. This is usually only necessary for those who have had two or more miscarriages.
What Can Cause Miscarriages?
Warnings
- If your pregnancy is past the 20-week date, and you experience heavy bleeding or cramping, go to the hospital right away. A pregnancy that terminates after this date is called a stillbirth.⧼thumbs_response⧽
References
- ↑ http://americanpregnancy.org/pregnancy-complications/miscarriage/
- ↑ Rebecca Levy-Gantt, MPT, DO. Board Certified Obstetrician & Gynecologist. Expert Interview. 3 April 2020.
- ↑ Rebecca Levy-Gantt, MPT, DO. Board Certified Obstetrician & Gynecologist. Expert Interview. 3 April 2020.
- ↑ http://www.plannedparenthood.org/learn/pregnancy/miscarriage
- ↑ http://www.plannedparenthood.org/learn/pregnancy/miscarriage
- ↑ http://americanpregnancy.org/pregnancy-complications/miscarriage/
- ↑ Rebecca Levy-Gantt, MPT, DO. Board Certified Obstetrician & Gynecologist. Expert Interview. 3 April 2020.
- ↑ http://www.whattoexpect.com/pregnancy/symptoms-and-solutions/vaginal-discharge.aspx
- ↑ http://www.plannedparenthood.org/learn/pregnancy/miscarriage
- ↑ http://americanpregnancy.org/pregnancy-complications/miscarriage/
- ↑ http://americanpregnancy.org/pregnancy-complications/miscarriage/
- ↑ http://www.plannedparenthood.org/learn/pregnancy/miscarriage
- ↑ http://www.babycentre.co.uk/a1039515/understanding-early-miscarriage
- ↑ http://americanpregnancy.org/pregnancy-complications/miscarriage/
- ↑ http://americanpregnancy.org/pregnancy-complications/miscarriage/
- ↑ Rebecca Levy-Gantt, MPT, DO. Board Certified Obstetrician & Gynecologist. Expert Interview. 3 April 2020.
About This Article
To determine if you had a miscarriage, watch for heavy vaginal bleeding and cramps similar to when you have your period, which are the most common symptoms. Another thing to look out for is pink or white vaginal mucus, which may also contain pregnancy tissue. If you experience moderate to severe lower back pain, consult your doctor, since you could be having a miscarriage. Pay attention to how you feel as well, since reduced morning sickness or less swelling in your breasts may indicate a miscarriage. If you think you've had a miscarriage, make sure to call your doctor right away, who may advise you to go a local emergency room for treatment. For tips on how to identify different types of miscarriage, keep reading!