This article was co-authored by Marc Kayem, MD. Dr. Marc Kayem is a board certified Otolaryngologist and Facial Plastic Surgeon based in Beverly Hills, California. He practices and specializes in cosmetic services and sleep-related disorders. He received his Doctorate in Medicine from the University of Ottawa, is board certified by the American Board of Otolaryngology, and is a Fellow of the Royal College of Surgeons of Canada.
There are 21 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 80% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 294,077 times.
More than 18 million people in the Unites States suffer from some form of sleep apnea.[1] The two primary forms of sleep apnea include central sleep apnea and obstructive sleep apnea. The majority of people suffer from obstructive apnea. Diagnosis is simple but inconvenient, as most people will be need to undergo a sleep study to confirm the diagnosis and severity of the apnea. Once diagnosed, the available treatment options are effective and often do not require the use of any medications.
Steps
Differentiating Obstructive Sleep Apnea from Central Sleep Apnea
-
1Recognize the cause of obstructive sleep apnea. Obstructive sleep apnea is far more common than central apnea, and is most often caused by direct interference with the passage of air when your throat muscles relax, resulting in interrupted breathing.[2]
- The muscles in your throat support structures in your mouth and throat that normally remain open to let air pass through, even when you are sleeping.
- The structures supported by the muscles in your throat include the soft palate, the uvula, the tonsils, and the tongue.
- When the throat muscles relax too much as you fall asleep, your air passages are blocked.
- This causes a 10 to 20 second lapse of time when the level of oxygen in your blood is inadequate for the amount your brain needs.
- Your brain wakes you up briefly in order to restore the passage of air. In many cases, the person does not remember waking up.
- This can occur as often as 5 to 30 times every hour, or even more, and continues throughout the night.
-
2Recognize the symptoms. Some symptoms of obstructive sleep apnea may overlap with those of central apnea. In most people, the cause of the problem clearly indicates one of the two possible types. Common symptoms that occur with obstructive sleep apnea include the following:[3]
- Excessive daytime sleepiness that may cause you to fall asleep at work, while watching television, and have trouble staying awake to drive.
- Loud snoring, often loud enough to disturb the sleep of others, and is the loudest when you are positioned on your back.
- Observed episodes of periods of time when breathing stops.
- Waking up suddenly with a feeling of shortness of breath, often accompanied by a snorting, choking, or gasping sound.
- Waking up with a headache and/or chest pain.
- Difficulty concentrating during the day.
- Moodiness or noticeable changes in mood.
- Problems with insomnia, such as being able to stay asleep at night.
- Having high blood pressure.
Advertisement -
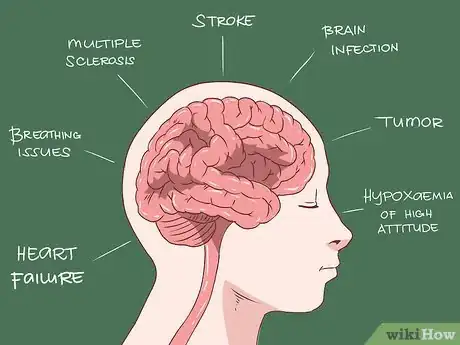
3Identify the causes of central sleep apnea. While the symptoms are similar, the underlying possible causes of central sleep apnea are different.[4]
- Central sleep apnea occurs when the brain sends faulty signals to the muscles responsible for regulating your breathing.[5]
- Central sleep apnea is much less common than obstructive sleep apnea and is usually related to another medical condition.[6]
- The most common causes for central sleep apnea are medical problems associated with serious cardiovascular problems such as heart failure, disorders that involve abnormal functioning of your brainstem, or a history of a stroke.[7]
- Some medications used repeatedly or in large doses can cause this type of sleep apnea. Opiates are the most common medications tied to causing central sleep apnea, as they send messages to the brain that disrupt and slow normal breathing patterns.
- Opiates that have been associated with central sleep apnea include morphine, oxycodone, and codeine.
-
4Note the symptoms of central sleep apnea. While the symptoms are similar and overlap with those of obstructive apnea, there are some differences. Symptoms associated with central sleep apnea include the following:[8]
- Shortness of breath that wakes you from sleep.[9]
- Shortness of breath that is relieved by changing your position to sitting upright.
- Observed periods of abnormal breathing, including periods when you stop breathing, while you are sleeping.
- Difficulty staying asleep often considered to be insomnia.
- Excessive daytime sleepiness that may cause you to fall asleep at work, watching television, or even driving.[10]
- Daytime evidence of poor sleep including difficulty concentrating, morning headaches, and mood changes.
- Snoring. Although snoring is also a symptom of obstructive apnea, it can also be unrelated to apnea.
Treating Your Sleep Apnea with Lifestyle Changes
-
1Implement lifestyle changes. Treatment options often begin with adjusting factors that may be within your control.[11]
- Seek medical attention to confirm your diagnosis and get support for the important lifestyle adjustments you can alter to help treat your apnea.
-
2Avoid alcohol use, especially daily or excessive use.[12] Alcohol significantly slows your rate of breathing. This causes the amount of oxygen that is available in your blood to be lower than normal. When you experience symptoms associated with sleep apnea, you want as much oxygen as possible to reach your brain.[13]
- Do not consume alcohol within four hours of your bedtime.
-
3Stop smoking. People that smoke will have more trouble with their air flow and airway passages.[14]
- Talk to your doctor if you need help to stop smoking. Products are available both over-the-counter and by prescription that can help you successfully quit smoking.
-
4Lose weight. If you are overweight or obese, this may be the primary cause of your sleep apnea.[15]
- Take steps to manage your weight in order to control your symptoms.
- Talk to your doctor if you need help with weight loss. Prescription products may help, plus your doctor can connect you with a nutritionist and possibly an exercise therapist to help you as you work towards your weight loss goal.
-
5Review your medications with your doctor. Be sure you doctor is aware of the problems you having with your sleep apnea.[16]
- With your doctor’s help, your routine medications can be adjusted to prevent them from aggravating your condition or causing problems.
-
6Sleep on your side. Try to avoid sleeping on your back to prevent snoring.[17]
- Use extra bed pillows to provide support against your back and help prevent you from rolling onto your back during your sleep.
- Special pillows are available to help you rest comfortably while providing support to help you sleep on your side.
-
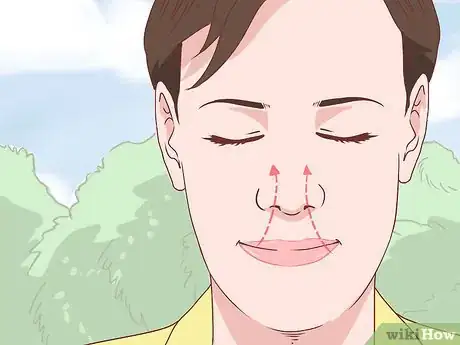
7Keep your nasal passages open. When you are congested or your nasal passages are blocked, this causes you to breathe through your mouth at night possibly triggering or worsening the apnea.[18]
- Talk to your doctor about the safest and most effective way to keep your nasal passages open at night. Over-the-counter products, including some that do not contain any medication such as breathing strips, are available.[19]
- Other products like saline nasal sprays or neti pots may work well for you to help your nasal passages stay clear at night.[20]
-
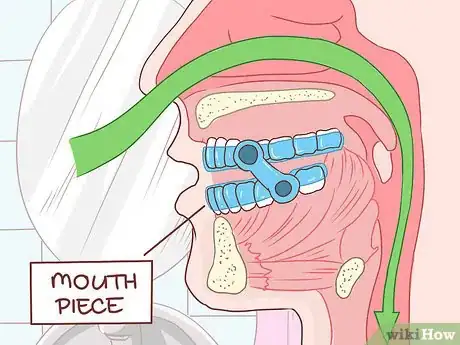
8See your dentist. Custom-fitted mouth devices are available specifically for sleep apnea.[21]
- The devices are made to fit in your mouth to keep your lower jaw and tongue in a position that keeps your airway passages open so you can breathe at night.
- This type of device may or may not correct the type of problem you have that is causing your apnea, so talk to your doctor first to determine if this may be helpful.
-
9Take steps to correct the underlying problem.[22] With the help of your doctor, you may be able to pinpoint the exact cause of your apnea.[23]
- For example, if you know that your tonsils are enlarged and are causing your apnea, then talk to your doctor about possible procedures to correct the problem.[24]
- In people that are suffering from central sleep apnea caused by cardiovascular issues, working closely with the cardiologist to address and correct those problems can help to reduce the symptoms of their apnea.[25]
- The same is true for people with diabetes. Taking good care of your diabetes, including steps to control weight management, can help to manage the sleep apnea symptoms.[26]
Treating Your Apnea with CPAP Equipment
-
1Clarify your diagnosis. To proceed with apnea treatment using CPAP equipment, which stands for continuous positive airway pressure, your diagnosis will likely need to be confirmed.[27]
- The method used to diagnose sleep apnea is a polysomnography test, most commonly referred to as a sleep study.
- This is inconvenient but necessary to confirm the diagnosis, determine the severity of your apnea, and is usually required to support the diagnosis by your insurance company so they will assist in paying for the equipment.
-
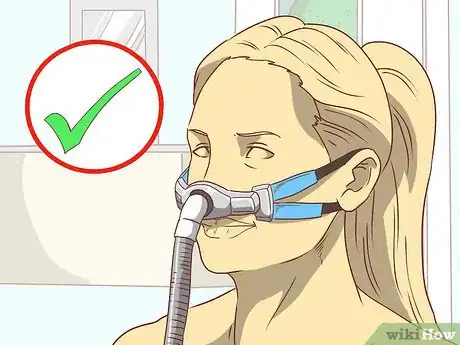
2Proceed with CPAP treatment. Once you have completed your sleep study, your doctor will explain the differences in the available equipment.[28]
- A CPAP unit provides a steady stream of air with enough pressure to prevent the tissues in your mouth and throat area from closing or collapsing as you sleep.
- Most units deliver a constant flow of air at the desired pressure level, which is adjustable and indicated on the machine.
- A newer method of delivering air pressure is called autotitrating positive airway pressure, or APAP. This type of unit adjusts automatically to the different breathing patterns of the person throughout the night.
- Many people describe the APAP equipment as being easier to get accustomed to and easier to tolerate.
- Some units available are called bilevel positive airway pressure, or BPAP. This type of unit is designed to deliver one level of pressure when the person is inhaling and another pressure level when exhaling.
- The most common CPAP unit weights about 3 pounds, has a tube that connects to the mask, and is compact enough to sit on your bedside table.
- The units have adjustable levels of pressure so you can begin with a small amount of pressure as you get used to the equipment, then gradually increase the pressure to the level your doctor recommended.
-
3Select the mask that suits your needs. Masks are available in different styles and sizes.[29]
- Some masks fit just over the nose and others are designed to fit over the mouth and nose.
- Try on several to determine the size and style that is most comfortable to you.
-
4Adjust the fit. Be sure the doctor or technician shows you how to adjust the fit of your mask.
- A mask that fits poorly can cause skin irritation, sores, and may not function as it is intended.
-
5Get accustomed to CPAP. It may be helpful to wear the mask for a few hours during the day without being attached to the actual unit.[30]
- Start with wearing the mask for fewer hours each night if you have trouble adjusting to it. Work towards keeping the mask in place with the unit on for the duration of your sleep time.
- Start with lower levels of pressure and gradually increase to reach the amount of pressure your doctor recommended.
-
6Wear the mask every night. Your sleep apnea is not being treated if you do not wear the mask with the appropriate amount of pressure. It is important that you wear your mask every night.[31]
- Additionally, it is very important that you give yourself a 1 to 3 month time frame to become used to wearing the mask every night. If you wake up and find you have removed your mask or headgear, put it back on and continue to sleep. This is an imperative part of creating the habit of sleeping properly with your CPAP.
- Consider that more than 80% of sleep apnea sufferers discontinue using their CPAP within the first year due to not forcing themselves to create the habit of wearing the CPAP mask. Unfortunately, they may not realize the dire health consequences they could be facing, such as a heart attack, by not making this important life change.
- Wear the mask for at least 6 to 7 hours each night for the best results.
- Most masks are designed with convenient travel cases so you can take it with you on business or pleasure trips away from home.
-
7Keep your unit clean. Clean and maintain your equipment, including your mask, every day.[32]
- Many units are equipped with computer chips that communicate the results of your sleep to your doctor. Follow your doctor’s instructions regarding the recorded information from your unit. Some units require that the chip be taken to your doctor’s office or downloaded via a computer.
-
8Address any problems. The most common complaints of CPAP users include simple side effects that can be managed.[33]
- Nasal congestion and dry mouth are common side effects. Many units are now equipped with built in humidifiers that help with these problems.
- Wear the chin strap that comes with your unit to prevent dry mouth. The chin strap functions to keep your mouth closed at night so you are breathing only through your nose.
-
9Consider surgery. Depending on your response to CPAP treatment, your success with recommended lifestyle changes, and the underlying cause of your apnea, surgery may be an option to consider.[34]
- Surgery is done to correct any problems related to anatomy and specific to the individual.
- Examples of surgical procedures sometimes used to treat sleep apnea include structural correction for nasal passage problems, excessive amounts of tissue in the soft palate area, or enlarged tonsils or adenoids that are blocking the passage of air when you sleep.
- If surgery is determined to be an option, the procedure done will be designed specifically to correct problems associated with that individual. There is no general surgical procedure performed that is universally used to correct sleep apnea.
Considering Risk Factors and Complications
-
1Become familiar with risk factors related to obstructive apnea. While anyone can have obstructive sleep apnea, some conditions and characteristics make the condition more likely to develop. The more common risk factors include the following:[35]
- Being overweight. As many as 50% of the people with obstructive sleep apnea are overweight. Fatty tissue deposits around the upper airway passages are thought to contribute to the problem.
- Having a larger waist size. While this factor is unclear as to the direct relationship to obstructive sleep apnea other than being overweight, it is considered a risk factor.
- Having a neck circumference greater than 17 inches in men, and 16 inches in women is associated with developing obstructive sleep apnea.[36]
- Being hypertensive, or having high blood pressure.
- Having a narrowed airway in your throat. This may be due to genetics or you may have enlarged tonsils or adenoids that are blocking the passage of air.
- Being diabetic. People with diabetes are more likely to have obstructive sleep apnea.
- Being a man. Men are twice as likely as women to develop obstructive sleep apnea.[37]
- Being black and under the age of 35. In this age group, obstructive sleep apnea occurs more often in black people.[38]
- Being between the ages of 18 and 60. While this disorder can occur in anyone at any age, it is more common in people that are between the ages of 18 to 60.
- Having a family history of obstructive sleep apnea places you at greater risk of developing the disorder.
- Being a smoker. Smoking puts you at higher risk of developing the disorder.[39]
- Drinking alcohol. Alcohol use tends to cause the symptoms to worsen.
- Being a woman past menopause. Women who are past menopause have a higher risk of developing sleep apnea.[40]
-
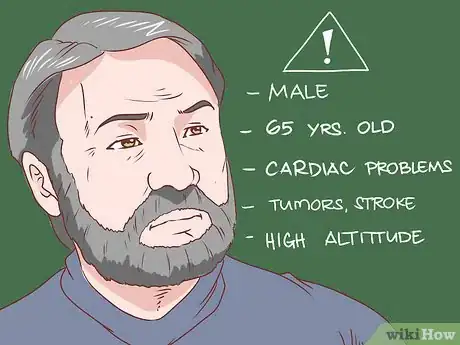
2Recognize risk factors of central sleep apnea. There are factors that increase your odds of developing central sleep apnea. While anyone can develop central sleep apnea, some factors clearly increase the risk. Some of the more common risk factors include the following:[41]
- Males are more likely to develop this form of sleep apnea.
- Adults over the age of 65 develop central sleep apnea more frequently, possibly due to other medical conditions or natural changes in sleep patterns.
- Cardiac problems including atrial fibrillation and congestive heart failure are often linked to central sleep apnea.
- Brain tumors, a history of stroke, and conditions that involve the brainstem are associated with an increased risk of developing central sleep apnea.
- Sleeping at high altitudes may contribute to central sleep apnea. This tends to resolve once you relocate to lower altitudes.
-
3Realize the complications of both types of sleep apnea. Both obstructive and central sleep apnea can lead to complications, with the possibility that some complications may develop even if you are treated.[42]
- It is not uncommon for some people to suffer from both forms of sleep apnea, or have one type develop after the first has been identified.
- The sudden changes in oxygen flow to the brain and other vital organs place a strain on the cardiovascular system. Consequently people may develop problems with high blood pressure which increases the risk of heart disease.
- Severe symptoms can lead to more serious consequences including coronary artery disease, heart attack, heart failure, cardiac arrhythmias, and stroke.[43]
- In people that already have a heart condition, repeated episodes of low blood oxygen can cause a sudden cardiac event and possibly death.
- Daytime fatigue can be overwhelming and can cause problems with functioning. Due to the frequent awakenings, your body is unable to establish the level of sleep needed, called restorative sleep, in order to be alert and well-rested during the day.
- People with obstructive or central sleep apnea are more likely to have problems with daytime concentration, memory problems, and mood changes.
- Some research has found a greater incidence of glaucoma in people that have obstructive sleep apnea.
- Another, but very important matter, is the disrupted sleep of your bed partner.
- Be sure your doctor or surgeon is aware of your condition in case you need a surgical procedure. The use of anesthesia can sometimes worsen symptoms for a short time following the procedure.
- Let your doctor know of your problems. Depending on your situation, some medications may need to be avoided that can cause further problems due to your sleep apnea.
Expert Q&A
-
QuestionWhat are some ways you can treat sleep apnea naturally?
 Marc Kayem, MDDr. Marc Kayem is a board certified Otolaryngologist and Facial Plastic Surgeon based in Beverly Hills, California. He practices and specializes in cosmetic services and sleep-related disorders. He received his Doctorate in Medicine from the University of Ottawa, is board certified by the American Board of Otolaryngology, and is a Fellow of the Royal College of Surgeons of Canada.
Marc Kayem, MDDr. Marc Kayem is a board certified Otolaryngologist and Facial Plastic Surgeon based in Beverly Hills, California. He practices and specializes in cosmetic services and sleep-related disorders. He received his Doctorate in Medicine from the University of Ottawa, is board certified by the American Board of Otolaryngology, and is a Fellow of the Royal College of Surgeons of Canada.
Sleep Specialist One way to avoid snoring with sleep apnea is by sleeping on your side rather than your back.
One way to avoid snoring with sleep apnea is by sleeping on your side rather than your back. -
QuestionWill sleeping with a fan on help me with sleep apnea?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician No, the problem with with your airway. You need positive pressure ventilation to help keep the airway open while you are sleeping.
No, the problem with with your airway. You need positive pressure ventilation to help keep the airway open while you are sleeping. -
QuestionIs it expensive to treat sleep apnea?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician It can be. CPAP machines are expensive and, if not covered by your health insurance, the price can be burdensome.
It can be. CPAP machines are expensive and, if not covered by your health insurance, the price can be burdensome.
References
- ↑ http://sleepfoundation.org/sleep-disorders-problems/sleep-apnea
- ↑ https://my.clevelandclinic.org/health/diseases/8718-sleep-apnea
- ↑ https://medlineplus.gov/ency/article/000811.htm
- ↑ https://www.sleepapnea.org/learn/sleep-apnea/central-sleep-apnea/
- ↑ https://medlineplus.gov/ency/article/003997.htm
- ↑ https://www.acc.org/latest-in-cardiology/articles/2014/07/22/08/25/basics-of-central-sleep-apnea
- ↑ https://medlineplus.gov/ency/article/003997.htm
- ↑ https://www.sleepapnea.org/learn/sleep-apnea/central-sleep-apnea/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2287191/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2287191/
- ↑ https://www.winchesterhospital.org/health-library/article?id=20180
- ↑ Marc Kayem, MD. Sleep Specialist. Expert Interview. 24 October 2019.
- ↑ https://www.helpguide.org/articles/sleep/sleep-apnea.htm
- ↑ https://www.helpguide.org/articles/sleep/sleep-apnea.htm
- ↑ https://www.winchesterhospital.org/health-library/article?id=20180
- ↑ https://www.helpguide.org/articles/sleep/sleep-apnea.htm
- ↑ https://www.winchesterhospital.org/health-library/article?id=20180
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/sleepapnea/treatment
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/sleepapnea/treatment
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/sleepapnea/treatment
- ↑ https://my.clevelandclinic.org/health/treatments/21129-oral-appliance-therapy-for-sleep-apnea
- ↑ Marc Kayem, MD. Sleep Specialist. Expert Interview. 24 October 2019.
- ↑ https://www.sleepfoundation.org/insomnia/what-causes-insomnia
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/003997.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/003997.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/003997.htm
- ↑ https://www.nhs.uk/conditions/sleep-apnoea/
- ↑ https://www.nhs.uk/conditions/sleep-apnoea/
- ↑ https://my.clevelandclinic.org/health/treatments/22043-cpap-machine
- ↑ https://www.helpguide.org/articles/sleep/sleep-apnea.htm
- ↑ https://www.helpguide.org/articles/sleep/sleep-apnea.htm
- ↑ https://my.clevelandclinic.org/health/treatments/22043-cpap-machine
- ↑ https://my.clevelandclinic.org/health/treatments/22043-cpap-machine
- ↑ https://www.uofmhealth.org/conditions-treatments/brain-neurological-conditions/surgical-alternatives-cpap
- ↑ https://healthysleep.med.harvard.edu/sleep-apnea/what-is-osa/risk-factors
- ↑ https://healthysleep.med.harvard.edu/sleep-apnea/what-is-osa/risk-factors
- ↑ https://healthysleep.med.harvard.edu/sleep-apnea/what-is-osa/risk-factors
- ↑ https://emedicine.medscape.com/article/295807-overview#a4
- ↑ https://emedicine.medscape.com/article/295807-overview#a4
- ↑ https://emedicine.medscape.com/article/295807-overview#a4
- ↑ https://www.uptodate.com/contents/central-sleep-apnea-risk-factors-clinical-presentation-and-diagnosis
- ↑ https://my.clevelandclinic.org/health/diseases/8718-sleep-apnea
- ↑ https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-dangers-of-uncontrolled-sleep-apnea
About This Article
If you've noticed signs of sleep apnea, including excessive daytime tiredness, loud snoring, or waking up and feeling short of breath, contact your doctor to confirm your diagnosis. In the meantime, try treating your sleep apnea with lifestyle changes, like sleeping on your side instead of your back, and using saline nasal sprays or a neti pot to keep your nasal passages open. You’ll also want to avoid alcohol and smoking, which can limit your breathing, and maintain a healthy weight. For more tips from our Medical co-author, including how to use CPAP equipment to treat your apnea, keep reading!








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...