This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 66,148 times.
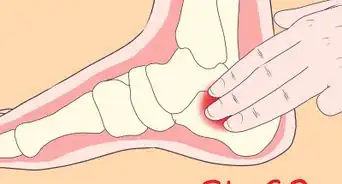
Metatarsalgia is a common and often painful condition resulting from inflammation in the ball of your foot. It’s a common issue among athletes, older people, and those who wear unsupported footwear, but it's generally very treatable. Often, resting the foot, applying ice packs to any swelling, and using over-the-counter anti-inflammatory pain medications can help treat any immediate pain. Long-term management is often possible by switching to low-impact exercises, dieting to maintain a healthy weight, and using supportive foot pads and inserts.
Steps
Caring for Metatarsalgia at Home
-
1Rest the affected foot. Minimize pressure on your foot and allow it to rest whenever you experience pain. Elevate your foot after any extended periods of standing or walking. Stop any physical activity if you notice it bringing on pain or making it worse.[1]
- You may need to avoid higher impact sports like running, basketball, football, or activities with a lot of jumping or impact while your foot heals. This can take anywhere from 10 days up to a few months. Opt for low-impact exercises such as swimming or cycling instead.
-
2Apply an ice pack to the affected area to reduce swelling and pain. Wrap a handful of ice in a towel or use a commercial ice pack and apply it to the pained area for 20 minutes at a time. Apply the ice pack any time you see swelling or feel pain. Just make sure to leave the ice pack off of your ankle for at least 30 minutes in between applications.[2]Advertisement
-
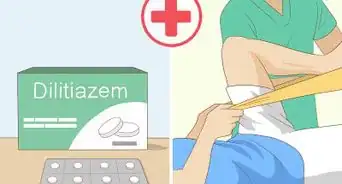
3Take ibuprofen to reduce pain. Over-the-counter pain medications such as ibuprofen can help minimize swelling and temporarily reduce pain. The recommended dosage for the average adult is 200 to 400 mg orally every 4 to 6 hours as needed. If you have any ongoing medical conditions or take other medications regularly, be sure to talk to your doctor prior to taking any new medications.[3]
- Other over-the-counter pain medications including naxopren and aspirin can also help manage metatarsalgia pain.
- Avoid long-term use of ibuprofen unless you're under the supervision of a doctor. If you are on other daily medications, including ACE inhibitors, talk to your doctor about potential drug interactions before taking any over-the-counter pain medication.
-
4Wrap your foot in a compression bandage. Help manage ongoing swelling and pain by wrapping your foot with a compression bandage. Start at the toes and work your way up the feet. If possible, ask your doctor, nurse, or physical therapist to show you how to properly wrap the bandage for the first time.[4]
- Your doctor may provide you with a compression bandage. If they don't, these bandages are readily available at most pharmacies and drug stores.
Treating Metatarsalgia Through Lifestyle Changes
-
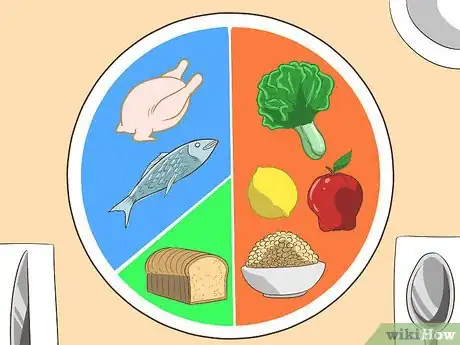
1Eat a balanced diet to maintain a healthy weight. Eating a healthy diet can help you achieve or maintain a healthy weight. This, in turn, takes pressure off your foot, helping to alleviate pain. Try to eat a balanced diet that is comprised of around 10-35% protein, 20-35% healthy fats, and 45-65% carbohydrates.[5]
- Try to focus your carb intake on complex carbs like fruits, beans, whole grains, and vegetables.
- Most of your diet should consist of anti-inflammatory foods. This includes foods like leafy greens, fresh vegetables, fruits, beans, fish, herbal teas, and olive oil.
-
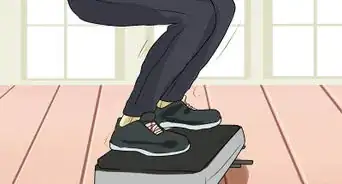
2Exercise regularly using low-impact training methods. Low-impact exercise helps maintain a healthy weight and restore a full range of mobility to your foot. While you recover, try exercises like walking, using an elliptical, swimming, cycling, rowing, yoga, and tai chi. Talk to your doctor or physical therapist to see how long you should maintain a low-impact exercise routine.[6]
- Some people need to stick to low-impact exercise for a few weeks to a few months after initially treating metatarsalgia. Others will need to switch to a low-impact routine for a matter of months, years, or even permanently.
-
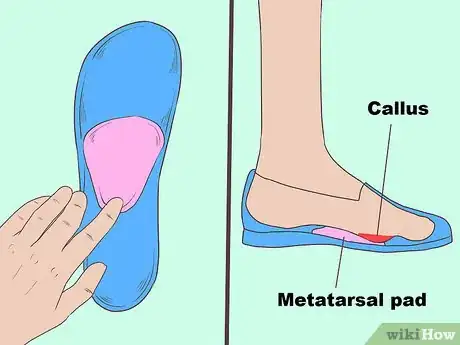
3Use metatarsal pads and arch supports in your shoes for continued support. Metatarsal pads and arch supports are available over-the-counter at most pharmacies and many shoe stores. Using these in your shoes on a daily basis can increase your support and minimize pain, especially if you walk or stand regularly as part of your job.[7]
- Insoles can also be custom fitted if you cannot find ones that work over-the-counter. If over-the-counter insoles do not help your pain or if they make matters worse, talk to your doctor about custom-fitted options.
-
4Switch your footwear to exercise shoes with cushioned soles. Wearing wider shoes with cushioned soles can help prevent future metatarsalgia-related pain. Switch your shoes to comfortable, cushioned styles and replace old shoes as soon as they wear down.
- Your doctor or podiatrist may be able to help you choose a brand of shoe that will work for your metatarsalgia. A shoe store that specializes in selling orthopedic and other specialty shoes may also be able to help you pick a comfortable pair.
- Try to avoid high heels as much as possible. Shoes with no arch support, such as flip-flops, can be used for short activities such as going outside to check the mail, but they should not be worn for longer periods of activity.
-
5Maintain a healthy weight. Carrying extra weight can worsen your symptoms of metatarsalgia. Since standing up puts twice as much pressure as your total body weight onto your foot, carrying extra weight can have a big impact on your feet. If you are overweight, it's a good idea to lose weight.
Seeking Medical Help
-
1Make a doctor’s appointment for any ongoing or worsening pain. Minor metatarsalgia can sometimes be treated at home with pain management and lifestyle changes. Pain lasting more than 2-3 weeks or worsening pain or swelling may necessitate a doctor’s visit. Your doctor or sports injury specialist can use x-rays, ultrasounds, or MRIs to look for complications and additional damage.[8]
- As metatarsalgia can often be treated at home, minor pains do not always require a doctor's visit or diagnosis. Ongoing or worsening pain, though, should be checked as soon as possible to make sure other conditions aren't responsible for or contributing to the problem.
- Problems like arthritis and bone degeneration can make metatarsalgia difficult to heal.
-
2Meet with a physical therapist who specializes in foot problems. If you continue to experience pain despite regular treatment, you may consider working with a physical therapist. Look for one that specializes in feet. If you are in the U.S., the American Physical Therapy Association website can help you find a specialist in your area.[9]
- Talk to your doctor about finding a physical therapist in your area. They can help you find one who will meet your specific needs. Check with your insurance, as well, as some providers may be covered under your healthcare plan.
-
3Ask your doctor if surgery is necessary. In rare cases, surgery may be necessary to treat metatarsalgia pain that cannot be relieved. If treatment is not working and your doctor has ruled out other potential causes for pain, talk to them about your surgical options. They will be able to review the surgical process and connect you with a specialist.[10]
- Depending on the cause and severity of your condition, potential surgeries may include hammertoe repositioning, bone repositioning, and bunion surgery. Recovery from these procedures could take 3-6 months.[11]
References
- ↑ https://www.mayoclinic.org/diseases-conditions/metatarsalgia/diagnosis-treatment/drc-20354795
- ↑ https://www.mayoclinic.org/diseases-conditions/metatarsalgia/diagnosis-treatment/drc-20354795
- ↑ https://www.drugs.com/dosage/ibuprofen.html#Usual_Adult_Dose_for_Pain
- ↑ http://marathontrainingacademy.com/how-to-self-treat-metatarsalgia
- ↑ http://blog.myfitnesspal.com/ask-the-dietitian-whats-the-best-carb-protein-and-fat-breakdown-for-weight-loss/
- ↑ https://www.nhs.uk/conditions/metatarsalgia/
- ↑ https://www.mayoclinic.org/diseases-conditions/metatarsalgia/diagnosis-treatment/drc-20354795
- ↑ http://www.sportsinjuryclinic.net/sport-injuries/foot-heel-pain/metatarsalgia
- ↑ http://aptaapps.apta.org/findapt/default.aspx?UniqueKey=



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...